All published articles of this journal are available on ScienceDirect.
Cervical Artery Dissection: Emerging Risk Factors
Abstract
Cervical artery dissection (CAD) represents an increasingly recognized cause of stroke and the most common cause of ischemic stroke in young adults. Many factors have been identified in association with CAD such as primary disease of arterial wall (fibrodysplasia) and other non-specific diseases related to CAD like Ehlers Danlos-syndrome IV, Marfan’s syndrome, vessel tortuosity. Moreover, an underlying arteriopathy which could be in part genetically determined, has been suspected. The rule of emerging risk factors for CAD such as recent respiratory tract infection, migraine and hyperhomocysteinemia are still a matter of research. Other known risks factors for CAD are major head/neck trauma like chiropractic maneuver, coughing or hyperextension injury associated to car. We examined emerging risks factors for CAD detected in the last years, as CAD pathogenesis is still not completely understood and needs further investigations.
EPIDEMIOLOGY
Cervical artery dissection (CAD) represents 20% of ischemic stroke in young adult under 45 years of age [1-3] and account for about 2% of all ischemic strokes [4-6].
Dissection of the carotid and vertebral arteries are rare, with a reported annual incidence of 2.5 to 3 per 100000 for carotid artery dissection [7] and an estimated annual incidence of 1 to 1.5 per 100000 for vertebral artery dissection (VAD) [8-10]. The increasing number of reported patients in recent years reflects both a growing familiarity with this complex clinical entity and a significant improvement in the methods of investigation. With aging, many other risk factors concurred to ischemic stroke, thus only 2-3% of all ischemic strokes are presumed due to CAD in elderly, but spontaneous CAD (sCAD) are often underdiagnosed in this population [11].
The reported incidence of sCAD may be underestimated cause the difficult to suspected and diagnose it in many conditions. In fact in stroke patients arterial dissection was the most relevant cause of headache [12] and in a recent study up to 8% of patients with sCAD presented headache or neck pain at stroke onset [13].
There are not prevalence among the sexes but it occurs approximately 5 years earlier in women than it does in men [8]. The predominant location of the dissections in the most mobile parts of the carotid arteries and VAs underscores the importance of a concomitant mechanical factor in the pathogenesis of sCAD. The occurrence of recurrent sCAD (sCAD) is rare and takes account of 3% to 8% in previous studies [6,9] and has been confirmed in a recent study with the evidence that delayed recurrence seems to be more common than previously suggested, and can occur at the level of the previously dissected vessel [14]. Among patients with spontaneous CAD, the reported risk of recurrent arterial dissection was 3% during an average follow up of 36 months [9] and reach 8% in a study with an average follow-up of 7,4 years, with the highest rate of recurrence (2%) within the first month after the initial event [6]. However, the incidence of CAD recurrences is difficult to assess because some recurrences are asymptomatic, especially within the first weeks [15] and dissections with isolated local signs are probably undiagnosed.
In a large multicentric study [16] the rate of symptomatic CAD recurrence is 0.3% per year and it is slightly lower than reported in previous studies [6, 9] in which patients with connective tissue disease or a familial history of CAD accounted for the vast majority of recurrences. In fact, Schievink found a rate of recurrence of dissection is 50% in patients with a family history of arterial dissection compared to 6% of patients with non familiar disease [17].
SEASONALITY
A seasonal pattern in the incidence of CAD was described, suggesting seasonality as an environmental factor leading to CAD [18]. Some Authors observed this seasonal pattern in 200 consecutive CAD patients referring to the Mayo Clinic from 1970-1990 [19]. The Authors observed a seasonal peak in October. The seasonal variation was substantial, with approximately 58% more patients suffering a cervical artery dissection in autumn than during other seasons. These results were also confirmed by a sub-analysis of patients living within 500 km of the same community (Rochester) in order to avoid the bias of the large climatic fluctuation occurring in Minnesota (USA) [20]. Numerous theories have been proposed to explain the seasonal variations in CAD including weather related changes in blood pressure, coagulation parameters, rheological factors, physical activities, diet and air pollution [21, 22]. Indeed, the seasonal variation of blood pressure is well known, with blood pressure being higher in cold seasons [23] because of a possible cold-induced peripheral blood vessel constriction [24].
However, it is not possible to exclude that cold seasons could favor upper respiratory infections and/or frequent sneezing and coughing thus being responsible for CAD. A recent story of respiratory tract infection due to Chlamydia Pneumonia has been found associated with CAD [18]. A recent study demonstrates mild seasonal variation in the occurrence of sCAD and recurrent sCAD with a peak in winter; in this study, seasonality was not found in patients with sVAD, but the lower number of patients in this group may have prevented the detection of significant results [25].
VASCULAR RISK FACTORS
In Western countries, < 5% of all strokes occurs in subjects <45 years of age, with a higher proportion between 19% -30% in developing countries. In young adults, a presumed premature atherosclerotic etiology, which affects larger extra and intracranial vessels is found in 20-25% principally due to classical risk factors (hypertension, diabetes, smoke, hyperlipidemia, hyperhomocysteinemia).
A potential link between conventional vascular risk factors has not been studied systematically [26] but various studies have measured the risk factors commonly associated with atherosclerosis, such as, hypertension, diabetes, smoking, oral contraceptive use or cholesterol levels. A recent case-control study found that hypertension was also significantly associated with sCAD and cerebral infarction [27]; Konrad and colleagues also found smoking and hypertension to be associated with dissection [28]. In another study, the presence of hypertension was associated with a lack of recanalization [29].
Baumgartner et al. observed a higher prevalence of hypercholesterolemia in patients with carotid artery dissection and ischemia, compared to those without ischemia; probably, the presence of hypercholesterolemia leads to a major endothelial subintimal damage and secondary occlusion [30]. A systematic review of risk factor for CAD reported that in general CAD was less likely to be associated with vascular risk factor than non-CAD ischemic stroke [31]. CAD ischemic stroke occurs in much frequency in adults younger than 45 years of age when the risk of atherosclerosis is modest, whereas, atherosclerosis increases exponentially with age when the risk of CAD is rare [8, 24, 28].
Hyperhomocysteinemia has also been associated with CAD as another risk factor [32, 33] and a strong association was found for homocysteine level >12 µmol /L [34]. Recurrence of cervical artery dissection is rare (0.3% risk per year) [35] compared to atherosclerotic diseases. The association between migraine and CAD is reported in various studies [36, 37].
Migraine is reported as an independent risk factor for dissection in a case-control study with a strong association among cases of CAD as compared to ischemic stroke not related to CAD, suggesting that the possible underlying arterial wall disease leading to dissection could be a predisposing factor for migraine [36]. However, the lack of multivariate analysis or the lack of blind assessment suggest prudence to the interpretation of this findings.
CONNECTIVE TISSUE ABNORMALITIES
The majority of cases the CAD are idiopathic. The question is why possible triggered movement of common daily life can cause cervical artery dissections. In this patients an underlying arteriopathy leading to a so called “weakness of the vessel wall” has often been postulated, especially if more than one cervico-cerebral vessel is involved and the patient is young: connective tissue abnormalities were present in 55% of patients whereas none of the non-CAD ischemic controls presented such abnormalities [38]. Ultrastructural abnormalities of arterial wall principally called fibrodysplasia is found in about 15% of patients with ischemic stroke and CAD. Is still matter of discussion if the deficit of α1-AT is associated to sCAD: Vila et al. found a strong association with low level of α1-AT [39] but larger and more recent studies did not confirm these data and found no differences in α1-AT genotypes between cases and controls [28, 40].
Other non-specific diseases related to CAD are Ehlers Danlos-syndrome IV (EDS type 4), Marfan’s syndrome, osteogenesis imperfecta type I [41], cystic medial necrosis of intracranial vessels [42], vessel abnormalities, and potential predisposing genetic conditions. Fibromuscular dysplasia is found in up to 20% of patients with CAD [43, 44]. It may be a non-specific entity that may also occur in Marfan's syndrome and cystic medial necrosis [45]. Fibromuscular dysplasia of renal arteries is also occasionally associated with CAD [46], suggesting a systemic pre-existing artery disease [47]; it may even lead to renal infarction [46]. The high incidence of dissection and cerebral aneurysm in patients with known hereditable tissue abnormalities such as EDS type 4 supported the hypothesis of an underlying connective tissue disorder leading to a structural instability of the arterial wall [38,48]. Although these well characterized heritable connective disorders have been identified, they have been found in only 1-5% of patients with CAD [48, 49]. The hypothesis is that the major part of sCAD cases represents a manifestation of a genetic predisposition in patients with a vascular phenotype [50]. Studies reported the existence of aberrations of collagen fibrils and elastic fibers within the reticular dermis type “EDS-like” or other ultrastructural abnormalities of connective tissue in more than half of patients with sCAD. The same Authors reported that only 1 out of 23 patients with traumatic CAD showed these aberrations suggesting a different pathogenesis for the two types of sCAD abnormalities [51, 52]. A relative diameter change (>11,8%) of common carotid artery during cardiac cycle was associated with dissection of internal carotid artery [53, 54], whereas aortic diameter larger than 34 mm was related to the dissection in another study. Genetic factors may also play a role in the pathophysiology of CAD, as part of a multifactorial predisposition [55]. Recent studies reported associations with different candidate genes: ICAM-1, COL3A1 and MTHFR [3, 56, 57]. The associations with the ICAM-1 E469K, and the COL3A1 3’UTR 2bp deletion polymorphisms have not been reproduced so far [58, 59]. The ongoing larger multicentre genetic association studies, such as the CADISP consortium, (www.cadisp.org) could provide much accurate information on this topic.
Redundant internal carotid arteries, bilateral redundancies and the number of redundant vessels were also identified as risk factors [60]. As endarterectomy is usually not used to treat sCAD and postmortem examinations are rare, the skin may serve as indirect approach to study possible connective abnormalities of the arterial wall [61].
CHIROPRACTIC MANIPULATION
Manual cervical spine manipulation is a therapeutic procedure that might result in cerebrovascular insults, primarily dissection of the vertebral artery (VAD) [62, 63]. This could be due to the anatomy of the vertebral artery: before the artery enters the skull base it winds around the atlas. The artery changes its direction from a vertical path to a horizontal path, at which point it is susceptible to injury from rotation and extension [62, 64, 65]. While the carotid artery lies freely in the soft tissues of the neck, it is more mobile and less vulnerable than the vertebral artery, but in some circumstances, it can be compressed against either the transverse processes or the bony mass of the upper cervical vertebrae during chiropractic manipulation.
The reported prevalence of dissection post trivial trauma in large cohorts of studies is between 12 to 34% [9, 66, 67]. The association between chiropractic manipulation and CAD has been reported in several studies [68, 69].
The first case of carotid artery dissection due to chiropractic manipulation was described in 1947 [70]. Some authors have suggested stroke rates ranging from one in 100.000 to one in 2.000.000 [71, 72]. In recent literature two studies on manipulation therapy were used as proxy for minor trauma. Smith et al. identified patients with dissection and vertebrobasilar stroke from a prospective stroke registry and assigned stroke aetiology in a blind and systematic method. The authors compared controls matched for age and sex, from the same registry and interviewed all subjects to determine the timings of both neck pain and cervical manipulation. Multivariate analysis was used in order to control the impact of important variables such as age, other stroke risk factors and neck pain prior to cervical manipulation. An approximately six-fold increased risk of cervical dissection and stroke/TIA was found. However, patients treated with cervical manipulation were younger even if they had been age and sex- matched than the controls [72]. Recently, a large case-control study in Ontario, Canada was not able to demonstrate any significant association between VAD or occlusion following manipulation in patients over 45 [73].
Approximately, 250 million chiropractic office visits are carried out yearly in the United States and another 25 million are carried out in Canada; 70% of these total North American visits are for cervical manipulation [71]. Considering this increasing utilization of manual manipulation, physicians need to be fully aware of the possible complication related to this therapy.
Since younger people are more likely to have dissection as a cause of stroke [69] and are more likely to visit a chiropractor [74] age should be considered as a possible confounding factor in the above-mentioned study.
Haldeman et al. reviewed 64 medicolegal cases of stroke following cervical manipulation: 92% of cases reported a history of headache and 25% complained about the sudden onset of unusual types of head and/or neck pain associated with other neurological symptoms such as dizziness or vertigo, nausea or vomiting, visual disturbance or tinnitus [75]. There was no relationship observed between the type of chiropractic manipulation and risk of stroke. Yet, there are several issues that remain to be resolved before it will be possible to estimate the risk of dissection after chiropractic manipulation. The authors found no relationship between type or number of manipulation and incidence of CAD: the stroke may occur after any type of manipulation technique including rotation, extension, lateral flexion and non-force and neutral position manipulation. A review of recent literature has not been able to determine what type of patients are at risk for these complications [76].
The problem is that the current data are often based on retrospective case-control data and selection and information bias were present. Therefore, caution is urged when attributing CAD to trivial trauma, as like as manipulative therapy, until further research is conducted [31].
In conclusion in the absence of randomized trials, the best current evidence suggests that cervical artery dissection, especially vertebral artery dissection should be considered as a random and unpredictable complication of any neck movement including cervical manipulation. Thus, a significant increase in pain, especially when associated with focal neurological signs following spinal manipulative therapy warrants immediate medical evaluation.
INFECTION
The association between recent infection and occurrence of artery dissection remains unclear. Recent infection has been suggested as a possible trigger of endothelial damage and artery dissection. Indeed, Grau et al. found a relationship between a recent history of infection and CAD comparing 43 patients with sCAD to 58 consecutive ischemic stroke patients younger than 50 years of age. Recent infection was more common in patients with CAD (58.1%) than in control patients (32.8%, p=0.01). However, the adjustment for the mechanical stress like coughing, sneezing or vomiting suggest only a weak association [18].
In a hospital-based case-control study Guillon et al. found a higher frequency of infection in patients with CAD (31.9%) compared to patients with ischemic stroke due to other causes (13.5%) [77]. This association was higher in patients with multiple dissections than in single dissection. However the limit of this study was that the presence of infection was assessed by questionnaire and no serological analysis was performed.
Direct vessel wall injury by a microbial agent and cellular infiltration seems unlikely [78, 79]. The role of indirect inflammatory and immunological host response, with activation of cytokines and proteases could induce excessive extracellular matrix degradation and thus weaken the vessel wall. It is also possible that an underlying structural defect of the arterial wall could be asymptomatic during the whole life and if infection is added the vessel wall could be damaged and influence the dissection. These structural defects are often underestimated. Indeed, Goldstein and colleague described a young adult whose carotid artery was found to have areas of previous, recurrent dissections, as well as an acute lesion necessitating excision of a pseudo-aneurysm. Although there was no angiographic evidence of an arterial anomaly, microscopic evaluation revealed underlying fibromuscular dysplasia [80, 81].
On the other hand, mechanical factors such as violent coughing, sneezing or vomiting associated with viral infection could be responsible for endothelial tear. This means that in case of infection the “minor trauma” could also be at the origin of CAD.
MAJOR CERVICAL TRAUMA
A history of different precipitating events characterized by movements of hyperextension or rotation of the neck is frequently reported in patients with CAD. CAD can be due to mayor head/neck trauma associated to car trash and hyperextension injury but it is very infrequent even with a severe head trauma [26].
Traumatic injury to the cervical spine and associated soft tissue structures occurs when these ranges are rapidly exceeded, as in trauma from high-speed motor vehicle accidents. The vertebral artery is frequently injured as a result of either stretching of the vessel over bone or direct injury from fractures involving the transverse foramen. Recognition of this injury at initial CT is essential, since affected patients may be asymptomatic. In contrast, injury to the carotid artery is uncommon and is more readily recognized due to clinical symptoms [82]
Vertebral artery Injuries due to major cervical spine trauma as determined by MR angiography are common. Although these vascular abnormalities usually remain clinically silent, a small rate of patients may present neurological deficits of stroke of posterior circulation. Noninvasive assessment of the vertebral arteries by means of MR imaging should be an integral part of the evaluation of the acutely injured cervical spine [83].
In Table 1 are shown various causes of dissections describe on case-reports published in the last thirty years.
Causes of Dissection Reported in Literature Case-Reports
| Reported association with CAD |
| Delivery and Pregnancy |
| Dental extraction of mandibular third molar |
| Violent coughing attack and vomiting |
| Sneezes |
| Oral contraceptives |
| Nose-blowing |
| Sexual Activity |
| Prolonged telephone usage |
| Yoga practice |
| Long standing star gazing |
| Emergency cardiopulmonary resuscitation |
| Beauty parlor stroke |
| Rap dancing |
| Chiropractic manipulation |
| Rigid Esophagography |
CONCLUSIONS
The available data encourages researchers to improve the understanding of the underlying pathophysiology and to focus on environmental as well as genetic risk factors of CAD.
Medical treatments and prevention strategies available are probably effective to modify the natural history of this disease. Whether the design of a randomized controlled trial is feasible, given the low incidence of CAD, is currently under appraisal.
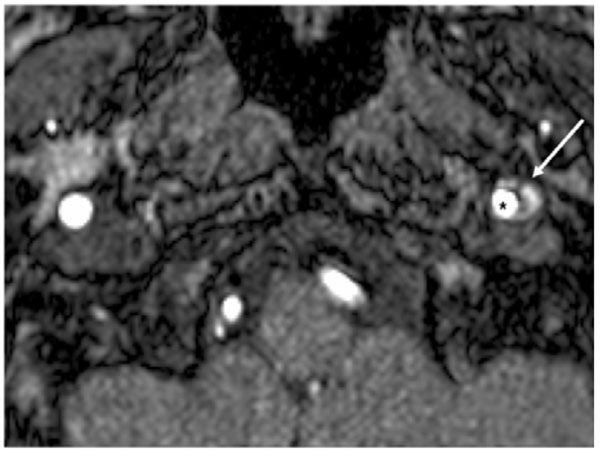
Axial magnetic resonance imaging scan showing a semilunar hyperintense signal due to the mural hematoma (white arrow) and an eccentric hypointense signal due to the residual lume, (black star).


