All published articles of this journal are available on ScienceDirect.
Clinical and Linguistic Profiles and Challenges in Diagnosis of Primary Progressive Aphasia in Medan, Indonesia: A Hospital-based Study
Abstract
Background
Primary Progressive Aphasia (PPA) is a degenerative condition characterized by progressive loss of language function. Studies on PPA patients in Indonesia are still limited, and none has reported clinical and linguistic profiles of PPA patients who speak Bahasa Indonesia.
This study aimed to describe clinical and linguistic profiles and challenges in the diagnosis of PPA patients from referral hospitals in Medan, Indonesia.
Methods
We retrospectively reviewed the clinical records of patients diagnosed with PPA based on the 2011 diagnostic criteria during the 2022-2023 period and described clinical characteristics data and linguistic profiles using descriptive analysis.
Results
We included 6 cases that fulfilled the diagnostic criteria for PPA. There were 3 cases categorized as nfvPPA, 1 case as svPPA, and 2 cases as lvPPA. There was female predominance (83.3%) and the mean age at onset was 59±2.96 years. The first symptom reported in the nfvPPA group was effortful, non-fluent speech; in svPPA, it was impaired naming and single word comprehension, while in lvPPA, it was impairment in word retrieval. Challenges in diagnosis included the availability of a standardized language tool aimed specifically for PPA in Bahasa Indonesia and the expertise needed to make such a diagnosis.
Conclusion
The main clinical features of the PPA reported were similar to previous findings with specific characteristics of Bahasa Indonesia. Determining language profiles of each variant of PPA in Bahasa Indonesia is crucial to establishing a correct diagnosis. Language assessment tool in Bahasa Indonesia is urgently needed to facilitate better assessment and management planning to improve quality of life.
1. INTRODUCTION
Primary Progressive Aphasia (PPA) is a group of clinical syndromes resulting from degenerative processes, characterized primarily by progressive language and/or speech impairments that are progressive. The main feature of PPA is a slow and isolated impairment in the use and comprehension of words. The diagnosis is established if other cognitive functions such as memory, visuospatial abilities, executive function, and behaviour remain relatively unaffected and if language is the sole affected domain for at least the first 2 years of the disease course [1, 2]. There are three variants of PPA including nonfluent variant (nfvPPA), semantic variant (svPPA), and logopenic variant (lvPPA). These variants can be distinguished based on the profile of speech and language impairments, supported by imaging findings of atrophy [3, 4]. The prevalence of PPA is relatively low compared to other neurodegenerative disorders, such as Alzheimer's disease. It is often considered a variant of Frontotemporal Lobar Degeneration (FTLD), although some cases are variants of Alzheimer's disease. The exact prevalence of PPA can vary based on the population, but estimates range from 3 to 20 cases per 100,000 individuals. Typically, PPA affects individuals in their mid-50s to early 60s, although it can occur at various ages [5]. Currently, there is no precise estimate of PPA frequency from population studies. However, rough estimates based on its most common cause, FTLD, range from 2.7-15 per 100,000 individuals, with annual incidence estimating around 2.2-3.5 per 100,000 individuals. The age of onset is estimated to range from the 50s, although it can affect individuals as young as their 20s or as old as 82 [2].
Similar to other degenerative dementias, early diagnosis of PPA is crucial and provides benefits for both patients and their families. Early PPA diagnosis is essential in clinical practice due to its complex and evolving phenotype. Moreover, accurate diagnosis is crucial to increase the likelihood of appropriate clinical interventions, especially in optimizing patients' communi- cation abilities and improving their quality of life. However, the clinical diagnosis of PPA is complex, and there is often a gap of several years between the onset of symptoms and the establishment of a PPA diagnosis [4, 6].
PPA diagnosis involves neuropsychological assess- ments covering a comprehensive language function examination. Several diagnostic instruments for PPA, including but not limited to assessments of naming ability, sentence production and comprehension, object know- ledge, repetition, reading, and writing skills, are available [7]. Most of these instruments are derived from English and cannot be directly applied to Indonesian-speaking PPA patients. The adaptation of language assessment instru- ments from English poses its challenges [8]. The most commonly used instrument for aphasia assessment by clinicians in Indonesia is the Tes Afasia untuk Diagnosis Informasi dan Rehabilitasi (TADIR). The test takes approximately one hour. The classification of aphasia based on TADIR refers to the Boston Diagnostic Aphasia Examination (BDAE), which reflects vascular aphasia syndromes and their anatomical correlations. However, as of now, there are no reported studies on the use of TADIR in PPA assessments [9]. Moreover, due to differences in their clinical features, the diagnosis of PPA variants remains challenging, and needs very high expertise and extensive experience of clinicians in assessing such patients. Studies on PPA in Indonesia are still limited, and data on the profile of Indonesian-speaking PPA patients are not well-documented. Therefore, data are needed to gain an understanding of the clinical characteristics and diagnostic challenges of PPA patients in Medan and improve patient management and treatment planning. We aimed to describe clinical and linguistic profiles and challenges in the diagnosis of PPA patients from referral hospitals in Medan, Indonesia.
2. METHODS
2.1. Study Design and Participants
We retrospectively reviewed the clinical records of patients diagnosed with PPA based on the 2011 diagnostic criteria) during the 2022-2023 period from two teaching hospitals in Medan, Indonesia, namely Adam Malik General Hospital and Universitas Sumatera Utara Hospital.
2.2. Procedures
The diagnosis of PPA was made by a neurologist specializing in behavioural neurology in accordance with the 2011 diagnostic criteria for PPA from the international consensus [3]. All patients underwent a structured neurocognitive examination, which consisted of the Montreal Cognitive Assessment Indonesian Version (MoCA-INA) and a language battery called TADIR or Tes Afasia untuk Diagnosis, Informasi dan Rehabilitasi. We collected demographic and clinical data for each patient. Demographic data consisted of age, sex, level of education, and occupation. Clinical data included cognitive and language profiles from the structured neurocognitive and language assessments. We also collected imaging data, which included structural Magnetic Resonance Imaging (MRI) and/or head computed tomography (CT) scans, and reported the peak atrophy site for each patient.
2.3. Data Analysis
Data are presented as mean value and standard deviation (SD) for normally distributed continuous variables, median (minimum–maximum) for continuous variables with a non-normal distribution, or frequency (%) for categorical variables. Data from this study were analyzed statistically using SPSS for Windows computer program (Statistics Products and Science Services) version 22.0. Statistical significance was set at p <0.05.
3. RESULTS
During the period of 2021 to 2023, there were 6 cases of PPA, consisting of 3 nfvPPA, 1 svPPA, and 2 lvPPA patients from 2 teaching hospitals in Medan. The mean age at onset and examination was 59±2.96 and 60±3.68 years, respectively. The characteristics of the subjects are presented in Table 1.
According to TADIR assessments, there were 2 patients with Broca aphasia, 2 patients with conduction aphasia, 1 patient with global aphasia, and 1 patient with Wernicke aphasia. The clinical and diagnosis of PPA are presented in Table 2.
All nfv PPA patients were presented with effortful and non-fluent speech. This was accompanied by the use of simplified sentence structures and a corresponding difficulty in comprehending grammatically complex expressions. Additionally, there seemed to be a motor disorder contributing to their laborious speech, namely Apraxia of Speech (AoS), which involved impaired coordination and planning of the motor articulators, leading to the production of incorrect speech sounds and sequences. Two out of three nfv PPA patients were classified under Broca's aphasia, according to TADIR, while one fell under global aphasia due to limited verbal output. When asked to describe daily activities to assess speech fluency, the patient tended to use nouns and did not use verbs or subjects. An example of a formed sentence was:
“Kalau habis bangun tidur bersih ini sprei biar cantik”
If after waking up (from sleep), clean this bedsheet so pretty (neat)
What she was trying to convey was that after waking up, she made her bed to keep it tidy. The patients also showed impaired comprehension. When assessed using TADIR, the patients had impairment in understanding the syntactically complex sentence. For example, for the question “Seorang bayi lebih besar daripada seorang dewasa. Benar atau tidak?” (A baby is bigger than an adult. True or false”), she answered true. In the sentence production test using pictures, she was asked to make a sentence from a picture, but she could only mention the objects and not make a sentence. The imaging results of one nfvPPA patient revealed atrophy in both frontal lobes, with more pronounced atrophy on the left side, as illustrated in Fig. (1).
SvPPA patient was presented with impaired naming and single-word comprehension. This patient had profoundly impaired naming ability, with frequent superordinate errors (e.g., naming “elephant” as “animal”) as well as coordinate errors (e.g., naming a “rhinoceros” as “horse). This patient had relatively preserved reading and writing abilities. Spontaneous speech exhibits fluency and verbosity but tends to lose substance over time, characterized by an increasing use of vague terms like “thing” and a limited reliance on specific nouns. The ability to repeat words remained relatively unaffected but with a lack of an understanding of their meaning. She also had difficulties in repeating longer sentences, especially those containing less common words, and difficulty comprehending the task of sentence repetition.
| Characteristic | Number (%) n= 6 |
|---|---|
|
Sex Male Female |
1 (16.7) 5 (83.3) |
| Age at onset, mean±SD (years) | 59±2.96 |
| Age at examination, mean±SD (years) | 60±3.68 |
|
Age group ≥50-59 ≥60-69 |
3 (50.0) 3 (50.0) |
|
Level of education High school University |
1 (16.7) 5 (83.3) |
| Duration of education, median (range), years | 15 (12-16) |
|
Occupation Housewife Retired Self-employed |
3 (50.0) 2 (33.3) 1 (16.7) |
| MoCA-INA score, mean±SD | 8.8±5.74 |
|
Subtype of PPA Nonfluent/agrammatic Semantic Logopenic |
3 (50.0) 1 (16.7) 2 (33.3) |
| Patient | Clinical Features | Diagnosis according to TADIR | Diagnosis according International Diagnostic Criteria | Peak Atrophy Site |
|---|---|---|---|---|
| 1 | Effortful, non fluent speech | Broca aphasia | nfv PPA | Left frontal |
| 2 | Fluent speech with comprehension impairment | Wernicke Aphasia | svPPA | Left anterior temporal |
| 3 | Word retrieval deficit, repetition impairment | Conduction aphasia | lvPPA | Left temporoparietal |
| 4 | Apraxia of speech, no meaningful verbal output | Global aphasia | nfv PPA | Left frontal |
| 5 | Effortful, non fluent speech | Broca aphasia | nfv PPA | Left frontal |
| 6 | Word retrieval deficit, repetition impairment | Conduction aphasia | lv PPA | Left temporoparietal |
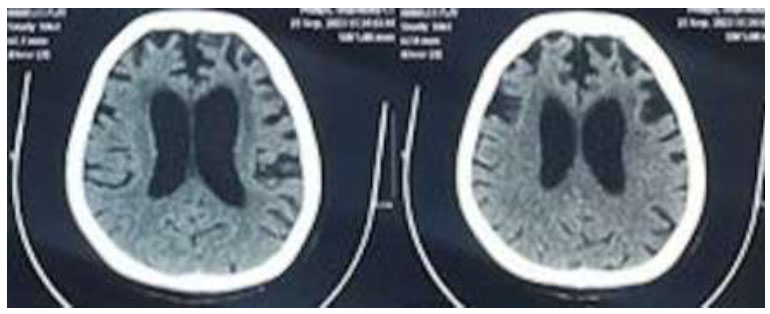
Imaging result of one nfvPPA patient.
LvPPA patients in our study were presented with word-retrieval difficulty and a slow rate of speech. They had significantly impaired sentence repetition with no evidence of agrammatism or speech articulation deficit and single-word comprehension. Word span was limited to a few short words, and only one long word. Naming errors in lvPPA manifested as phonemic paraphasia errors rather than semantic paraphasia. Verbal outputs were characterized by fluent islands with pauses, false starts, and hesitations. Unlike nfvPPA, verbal output is not effortful, and fluency is preserved, as measured by words per minute.
4. DISCUSSION
PPA syndrome is characterized by language impairment that emerges as the primary and sole symptom for at least the first two years after the onset of symptoms, remaining the dominant feature throughout the course of the disease [10, 11]. The onset of PPA typically occurs before the age of 65, with a relatively balanced prevalence between men and women [12]. We found that the mean age at onset was 59±2.96 years. This is similar to a previous finding that reported the mean age for disease onset is 59.6 years (SD 7.2) in svPPA, 64.4 years (SD 7.5) in nfvPPA, and 63.0 years (SD 7.9) in lvPPA [13] but lower than a study by Mouton et al. (2022) that reported a mean age of 73.1±9.1 years [7]. Female predominance was present in our study (83.3%).
Establishing a diagnosis of PPA requires a thorough examination focusing on early language impairment, gradual onset, and progressive deterioration in language skills. This includes assessing language production, object naming, syntax, and word comprehension through conversation or speech and language assessments. A comprehensive evaluation involving a detailed medical history and cognitive function assessment is crucial for diagnosing and determining the PPA variant. This process aims to confirm the diagnosis, plan tailored management, and consider potential progression [14, 15].
In our study, all patients underwent global cognitive assessment using MoCA-INA, which showed a lower-than-normal score in each patient. This finding is not surprising since it is a verbal-based tool and highly dependent on the patient’s verbal and language ability. We assessed language functions that included sentence production during spontaneous speech, word and sentence compre- hension, repetition, naming, reading, and writing to clinically classify each PPA variant. A key indicator in patients with PPA is the presence of asymmetrical damage to the cerebral hemisphere that is dominant for language function, manifesting as cortical atrophy, hypoperfusion, or hypometabolism. This illustrates the selective partial vulnerability of specific networks to neurodegenerative diseases [10]. Our study found the area of atrophy correlated well with the area known for each variant, namely left frontal in nfvPPA, left anterior temporal in svPPA, and left temporoparietal in lvPPA [3, 15].
The PPA case report from Indonesia is very limited. One study from Riswanto et al. reported a case of an older Indonesian person who claimed to have PPA and a behavioral variant of FTD. However, the main clinical symptoms reported were behavioral changes and memory problems, although she was also reported to have no speech ability [16]. The diagnosis of the PPA subtype in this study was based on the results of cognitive function assessments, particularly in the language domain, and structural imaging examinations, namely MRI and or Head CT Scan. The language assessment instrument used—TADIR—was not specifically designed for PPA, hence requiring specialized expertise for interpretation, including comprehensive knowledge of the correct structure of Bahasa Indonesia and related diagnostic criteria of PPA, which was originally developed in English, which poses several diagnostic challenges.
We will discuss the linguistic profiles of our PPA patients, compare them with previous studies on post-stroke aphasia in Bahasa Indonesia, and highlight differences in English for accurate PPA diagnosis. Additionally, we will address the challenges in diagnosing PPA in Bahasa Indonesia and evaluate the current language assessment tools for PPA and its variants.
The classification of aphasia based on TADIR refers to the Boston Diagnostic Aphasia Examination (BDAE), which reflects vascular aphasia syndromes. Therefore, to correctly classify PPA based on TADIR, the examining clinician must have comprehensive knowledge not only about its original interpretation but also of the diagnostic criteria of each variant of PPA [3]. All nfvPPA patients in our study were presented with simplified sentence production, which indicated the presence of agrammatism. Agrammatism in Bahasa Indonesia is primarily studied through post-stroke aphasia verbal output. Suhardiyanto outlined agrammatism in four Broca's aphasia patients, emphasizing simplified sentence structures as a key manifestation. While no distinct selective impairment in grammatical elements was noted, the production and use of grammatical words were unaffected. Notably, prepositions and conjunctions remained in patients' speech [17]. Agrammatism is characterized by disrupted verb retrieval and inflection. In Bahasa Indonesia, verb inflection is not used for internal and external sentence relationships; instead, free-standing morphemes are used. Agrammatic speakers face challenges in retrieving verbs and specifying event timeframes [18]. A previous study on 300 words from each participant's spontaneous speech identified agrammatic features such as slower speech rate, shorter mean length of utterance, and simpler sentence structures. Unique features included reduced derivational morphemes, normal inflectional morphemes, and proficient access to passive structures [19]. This aligns with Nasrullah's study on three Broca's aphasia patients, revealing irregular repetition, affixation elimination, lexical deficits, imperfect shapes, and syntactic function removal or exchange as verbal expression types [20].
Alongside grammar impairment in expression, individuals with nfvPPA also demonstrate difficulty comprehending complex syntax, including challenges with understanding embedded sentences featuring subordinate clauses. However, in the TADIR examination, no sentences with subordinate clauses appear in the middle of the sentence [9]. Therefore, this condition of comprehension impairment cannot be clearly evaluated only by using the existing tool. A previous study explored the understanding of passive structures in Bahasa Indonesia. Utilizing a sentence-to-picture matching task, the study examined four reversible sentence types (active, passive, subject cleft, and object cleft), incorporating variables such as word order, embedding, and relative frequency. Eleven participants with Broca's aphasia and agrammatic speech were involved. Findings indicated similar comprehension levels for both passive and active sentences, minimal impacts of embedding, and a more favourable understanding of subject clefts compared to object clefts. The identified deficit in sentence comprehension among individuals with Broca's aphasia in Bahasa Indonesia highlighted the importance of considering the frequency of syntactic structures [21].
Our study found one patient with nfvPPA classified under global aphasia according to the TADIR classification. The patient lacked meaningful verbal output but still employed gestures in an attempt to communicate. This is in line with previous research that revealed that individuals with global aphasia retained pragmatic abilities, expressing vocabulary and nonsensical sounds. They used gestures like nodding and hand movements, along with sudden intonation changes, mimicking sounds, and whispering to convey their intentions in speech [22].
In this study, there was only one patient with svPPA, and she presented with naming and single-word compre- hension impairments. While both poststroke aphasia and svPPA exhibit common language impairments such as anomia and single-word comprehension deficits, the underlying cognitive processes contributing to these issues differ. In poststroke aphasia, semantic errors in naming may stem from difficulties accessing semantics visually, damage to the semantic system, impaired access to lexical representations for output, or damage to an output buffer. Conversely, in svPPA, naming and comprehension are affected by the progressively degraded “object semantics” or “semantic memory.” In svPPA, the impairment in naming nouns surpasses that in naming verbs, while in nfvPPA, the pattern is reversed. Yet, in the naming subtest of TADIR, the distinction between nouns and verbs is absent; only nouns are considered, diminishing the visibility of this particular characteristic [12]. Our patient demonstrated relatively preserved reading and writing abilities. One characteristic of svPPA is surface dyslexia/dysgraphia [3, 23]. Surface dyslexia, which involves the regularization of words with unusual spellings, becomes apparent in reading. This condition leads to a phonological approach to reading, where the ability to recall the correct spellings of atypical words is compromised [12, 24]. This characteristic is not relevant to examine in Bahasa Indonesia, as words in Indonesian generally follow regular grapheme-phoneme conversion rules. This indicates that such linguistic features cannot be objectively assessed in Bahasa Indonesia.
Gorno-Tempini et al. (2004) contended that the fluency pattern observed in lvPPA does not align neatly with the traditional fluent/nonfluent classification employed in characterizing speech-language production in poststroke aphasias. In post-stroke aphasias, nonfluent aphasias typically involve slow, laborious speech production, modified prosody, omission of grammatical morphemes, and motor speech impairment. On the other hand, fluent aphasias are marked by phonological and lexical errors, normal speech rate, intact grammar, and unaffected motor speech production. In lvPPA, although motor speech and grammar remain intact, speech production is character ized by slowness and hesitation [23].
Classifying PPA can be challenging due to shared language characteristics, such as anomia, among its variants. Differential diagnosis is complicated by speech and language features that obscure distinctions, and there is variability in clinical presentation, particularly in nfvPPA and lvPPA. Resources offering explicit guidance for clinicians in assessing speech, language, and cognition in PPA, along with predicted performance on tests based on PPA variant, aid in diagnosis and classification [3, 12, 23]. Diagnosing PPA in Bahasa Indonesia is even more complicated by the absence of language assessment tools specifically designed to evaluate the linguistic profile of PPA and/or provide a final classification for PPA.
The main goal in diagnosing PPA is to plan effective management. However, the lack of a standardized battery for agrammatism diagnosis in Indonesia hinders the development of speech therapy guidelines. Studies indicate that derived word order is not crucial for treating agrammatic speech in aphasia patients. To improve, strategies should focus on the explicit production of relevant information, with training emphasizing pragmatic consequences of linguistic constructions in Bahasa Indonesia. Clinical implications stress caution in agram- matic aphasia therapy, ensuring emphasis on correct sentences doesn't compromise verb diversity. Speech therapy should prioritize diverse lexical verbs for effective daily communication [18, 19].
Our study had several limitations. We did not validate PPA subtype diagnoses through autopsy, and we acknowledge the imperfect sensitivity and specificity of existing clinical diagnostic criteria. There is a potential for overlapping symptoms and diverse underlying causes.
While our study benefits from a cohort of patients with a high level of education, we acknowledge that this demographic characteristic may restrict the generaliz- ability of our findings to the broader Indonesian population. Given that education level can influence health behaviors, access to healthcare, and treatment outcomes, our results may not fully capture the experiences of individuals with lower levels of education. To address this limitation, future research could aim to include a more diverse sample to ensure the robustness and applicability of our findings across different educational backgrounds.
Most importantly, the retrospective nature of our hospital-based study introduces bias in participant selection. This preliminary retrospective study serves as an initial exploration of this condition in Indonesia, which has the potential for extension in the future. We emphasize the need for future prospective studies across multiple sites or within the community to obtain more accurate epidemiological information on PPA in Indonesia.
CONCLUSION
In conclusion, this study sheds light on the clinical features of PPA within the Indonesian population, emphasizing the need for culturally and linguistically appropriate diagnostic tools. Through a retrospective analysis of patients presenting with aphasia symptoms, we provided insights into the linguistic and neurocognitive aspects of PPA, highlighting the challenges and opportunities for diagnosis and management in this context. While our study contributes to the understanding of PPA in Indonesia, several areas warrant further investigation. Future studies should aim to validate our findings through longitudinal assessments and include a more diverse sample to enhance the generalizability of results. Additionally, efforts to develop community-language usage diagnostic tools tailored to Bahasa Indonesia are imperative to improve early detection and intervention for individuals affected by PPA in this population. Overall, this study underscores the importance of addressing linguistic and cultural factors in the assessment and management of neurodegenerative conditions like PPA, ultimately aiming to enhance patient care and outcomes.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to itssubmission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AoS | = Apraxia of speech |
| BDAE | = Boston Diagnostic Aphasia Examination (BDAE) |
| lvPPA | = Logopenic variant Primary Progressive Aphasia |
| MoCA-INA | = Montreal Cognitive Assessment-Indonesian Version |
| MRI | = Magnetic Resonance Imaging |
| nfvPPA | = Non fluent variant Primary Progressive Aphasia |
| svPPA | = Semantic variant Primary Progressive Aphasia |
| PPA | = Primary Progressive Aphasia |
| SD | = Standard deviation |
| TADIR | = Tes Afasia untuk Diagnosis Informasi dan Rehabilitasi |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
We obtained ethical approval from the ethics committee Faculty of Medicine Universitas Sumatera Utara number 1123/KEPK/USU/2023.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki.
CONSENT FOR PUBLICATION
This is a chart review, and the ethics committee has waived patient consent.


