Vertebrobasilar Dolichoectasia Presenting Recurrent Episodes of Locked-in syndrome: A Case Report and Literature Review
Abstract
Introduction:
Vertebrobasilar Dolichoectasia (VBD) is a rare disorder in which arteries cause dilatation and tortuosity of the blood vessels, which affect posterior circulation.
Case Presentation:
In this case report, we discuss a patient of VBD presenting with transient episodes of quadriparesis, aphasia, and vertigo. She had symptoms specifically when her head was turned towards the right side while waking up. Based on MRI findings and angiography, the patient was diagnosed with VBD.
Conclusion:
To conclude, VBD should be considered a differential diagnosis for patients presenting with recurrent transient ischemic attacks, such as locked-in syndrome, without any identifiable cause.
1. INTRODUCTION
Vertebrobasilar dolichoectasia (VBD) is a rare disorder affecting posterior circulation. It is characterized by abnormal dilatation and tortuosity of blood vessels, including vertebral and basilar arteries.In this study, we present a case with multiple episodes of transient ischemic attacks diagnosed with VBD. The patient was found to have Medullary indentation by dilated basilar artery on MRI. This led to further workup and diagnosis of VBD. In addition, we also discuss key differentials and the utility of angiography in the diagnosis of this condition and discuss the treatment and follow-up of our patient.
2. CASE
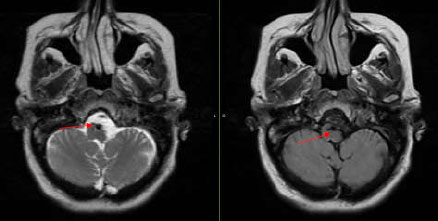
The patient, who presented with transient episodes of focal neurological deficits for six months, is a Caucasian female in her late 50s with a medical history of Hypertension and Diabetes. These episodes were wake-up weakness, confusion, and dysarthria on the right side of the body. She was prescribed Aspirin by a local neurologist. The episodes became more severe as she would have transient quadriparesis, dizziness, and aphasia lasting for several hours. These symptoms would happen particularly in the right lateral position. Her neurological exam was completely normal. CT scan head was normal, while CT Angiography revealed increased tortuosity of the V4 segments of the vertebral arteries and the basilar artery. These were indenting the Medulla oblongata. MRI brain confirmed similar findings (Fig. 1). A conventional angiogram was done, which revealed compression of the medullary pyramid on the left side due to dilated proximal basilar artery associated with significant vertebrobasilar atherosclerotic plaques (Fig. 2). No rate-limiting changes in flow were observed while turning the head to either side during the procedure, but approximately 50% flow arrest was seen in the right vertebral artery on turning the patient’s head to the right.
The patient was discharged on dual antiplatelet therapy and instructed to avoid sleeping on the right side. She continued to do well at three months follow-up. This case report has been exempted from IRB review by the University of Louisville Institutional ethics committee. (Ref. IRB 23.0025) Written informed consent was obtained from the patient for publication of the details of their medical care and any accompanying images. All authors approve and provide consent for publishing this work.
3. DISCUSSION
The estimated prevalence of VBD varies from 0.13% to 18% [1]. VBD is often detected as an incidental finding or diagnosed after symptoms develop due to compression of the brainstem or cranial nerves, ischemic strokes, or transient ischemic attacks [2, 3]. It can also present as a vascular event, most commonly ischemic stroke. It is important to identify VBD as this condition has been associated with a 17.6% risk of stroke, a 10.1% risk of transient ischemic attack, and a 4.7% risk of hemorrhagic stroke in a systematic review of 375 patients [4]. VBD also has an estimated 36.2% 5-year mortality risk [4].
VBD is suggested to be a vasculopathy. Often predisposing conditions like atherosclerosis, hypertension, and collagen vascular diseases preexist in such patients. Besides some genetic conditions, African American ancestry, Diabetes mellitus, Peripheral vascular disease, and smoking are considered potential risk factors [5, 6]. Internal elastic lamina damage is commonly seen finding on histopathology. Postulated mechanisms of this damage include an imbalance between matrix metalloproteinases and antiprotease activity within the vessel wall [7, 8]. This leads to defective connective tissue synthesis and abnormal vascular remodeling. It has been suggested that bidirectional flow from both vertebral arteries causes an increased risk of damage to the Basilar artery resulting in abnormal dilatation [9].
It is unclear how VBD increases stroke risk, but proposed mechanisms suggest stagnant flow leading to thrombosis or occlusion of perforating arteries [10]. Multiple case reports suggest brain stem compression can be associated with a higher risk of neurologic morbidity and mortality [11–14].
VBD can be diagnosed on CT angiography by the smoker criterion [15]. It considers the height of the basilar artery bifurcation and the lateral displacement of the basilar artery. If the height, as well as displacement, is more than the level of the third ventricle, and the diameter of BA is more than 4.5 mm, this qualifies as a diagnosis of VBD. MRI and MRA-based criteria have been developed based on this classification system [16]. These could be more sensitive due to better anatomical clarity.
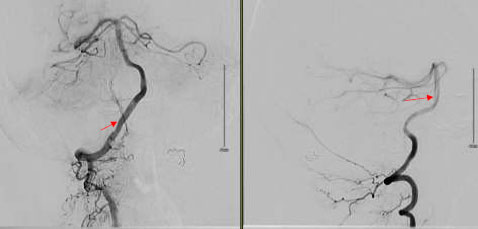
Cerebral angiography is the gold standard for the diagnosis of VBD. It can also help in deciding medical treatments versus endovascular intervention. Angiography was helpful in our case as it helped to quantify the severity of VBD. We were also able to rule out bow-hunter syndrome. Bow hunter syndrome results from mechanical compression of vertebrobasilar circulation on rotation or extension of the neck [17]. Due to significant atherosclerotic plaques seen in our patient, we managed her conservatively with dual antiplatelet therapy. Current evidence on the use of antiplatelet agents is limited to case series and anecdotal reports. In one of the case series, 79 out of 156 subjects were treated with antiplatelet agents, with a 1-year cumulative risk of stroke of 42% despite treatment [4].
Anti-thrombotic agents can also be used as a non-surgical treatment option for VBD, although no randomized trials are available [5, 18]. One of the studies suggested that warfarin use might be associated with a reduced risk of ischemic events, although the sample size was limited [5].
Surgical or endovascular therapy can be a good option if fusiform aneurysms are found in association with Dolichoectasia. The data on their utility in asymptomatic patients is not available [10, 19].
In our review of the literature, we could find one case report of the transient brainstem symptoms with VBD. The subject was in his 50s and presented with brain stem symptoms like dysarthria, dysmetria, nystagmus, and ataxia. He had dolichoectasia affecting both anterior and posterior circulation on MR angiography. This patient was treated with antiplatelet treatment, but follow-up was not available.
Our case report highlights that VBD can present with episodes of locked-in syndrome. VBD should be considered a differential diagnosis in patients with stroke-like symptoms when common causes cannot be identified. This is, however, an isolated case report, so there cannot be a generalization.
CONCLUSION
VBD is a rare condition associated with an increased risk of acute ischemic strokes and subarachnoid hemorrhage. VBD should be considered a differential diagnosis in patients with episodes of locked-in syndrome with unclear underlying diagnoses. Data on long-term treatment options for VBD is largely lacking. There is a need to systemically evaluate treatment options since it is associated with a high risk of mortality and morbidity.
AUTHORS’ CONTRIBUTIONS
Ayush Gupta prepared the script and collected available evidence. Talita Rosa contributed to the discussion section by providing additional evidence and supervising the preparation of the manuscript. Marwa Elnazeir conceptualized, edited, and supervised the case report and picked figures for the case.
LIST OF ABBREVIATIONS
| VBD | = Vertebrobasilar Dolichoectasia |
| CT | = Computed Tomography |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This case report has been exempted from IRB review by the University of Louisville Institutional ethics committee. (Ref IRB 23.0025).
HUMAN AND ANIMAL RIGHTS
Not applicable
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available upon request to corresponding author [M.E]. No separate data sets are available as this is only a case report, and imaging and angiography findings can be retrieved from the EMR and shared if requested.
STANDARDS OF REPORTING
CARE guidelines have been followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors acknowledge the patient for providing a learning opportunity on this rare disorder.


