All published articles of this journal are available on ScienceDirect.
The Relationship between Electroencephalography Recording Results and Magnetic Resonance Imaging Abnormalities and Drug Resistance Focal Epilepsy: A Comparative Analysis Study in Bandung, Indonesia
Abstract
Introduction
Drug-resistant Epilepsy (ERO) is a complex problem, both in diagnosis and management, and carries a high risk of death and risk of cognitive and behavioral problems. This study aims to determine the relationship between EEG recording results and structural abnormalities from MRI examination results in Drug-Resistant Epilepsy (DRE).
Methods
Quantitative comparative analysis was conducted to study focal epilepsy recorded in the pediatric neurology outpatient of Dr. Hasan Sadikin Hospital, Bandung, 2018-2023. Data collected from medical records included patient demographics and clinical data, EEG recording results, and MRI examination results. Data were subjected to Chi-square analysis with the alternative Fisher's exact test in SPSS 26. A p-value <0.05 was declared significant.
Results
From 67 samples, 34 DRE subjects and 33 drug-sensitive focal epilepsy (DSFO) subjects were obtained. More significant comorbidities were found in DRFO with a p-value of 0.027 and OR 8.88 (1.03-76.84). There was a significant difference in the results of EEG recordings in the two groups with p <0.001. The different EEG features were significant including slowing, polyspike, and frequency>1/60s. The MRI images were not found to be significantly different. The most common structural lesion found was focal cortical dysplasia in both groups. There was no correlation between MRI and EEG in DRE.
Conclusion
EEG recordings' results were better than MRI images' for predicting DRFO, including images of slowing, polyspike, and frequency >1/60. Both EEG and MRI had their respective values for predicting DRE.
1. INTRODUCTION
Epilepsy affects approximately 50 million people worldwide. It is estimated that 5 million people are diagnosed with epilepsy annually. In developed countries, the incidence of epilepsy is estimated at 49 per 100,000 people yearly. In low and middle-income countries, the incidence of epilepsy reaches 139 per 100,000 people yearly, and around 80% of people with epilepsy live in low and middle-income countries [1].
Drug-Resistant Epilepsy (DRE) remains a complex problem, both in diagnosis and management, and carries a high risk of death and risk of cognitive and behavioral problems [2-4]. The prevalence of DRE is approximately 30%, with an incidence varying from 15% in children to 34% in adults [1]. The onset of epilepsy in childhood has long-term consequences and impacts many aspects of a child's life, including at school, and later impacts on employment, marriage, and parenthood [3]. Besides the high risk of death, uncontrolled childhood onset of epilepsy can reduce cognition [4, 5]. The quality of parents' mental health of children with DRE is worse than that of parents of healthy children [6].
Risk factors significantly associated with DRE in research in Indonesia include early onset, symptomatic epilepsy, focal seizures, more than 1 type of seizure form, imaging abnormalities, unfavorable Electroence- phalography (EEG) evolution, and failure to control seizures early [7]. Drug-resistant epilepsy occurs more frequently at focal seizure onset than that of generalized seizure onset, and approximately 94% of focal seizures are associated with structural lesions [8]. One study in Egypt on cases of drug-resistant focal epilepsy (DRFE) found that the number of focal to bilateral epilepsy was relatively high at 79.7% [9].
Abnormalities in EEG results are important for the diagnosis of epilepsy. The activity of interictal epileptiform discharges can determine the focus of epilepsy. Apart from assessing the basic EEG waves, we also look for interictal epileptiform discharge activity in the form of sharp waves, spikes, and focal poly-spikes. Abnormalities in EEG results, such as persistent focal slowing or frequent focal epileptiforms, are considered prognostic markers of poor seizure control [10]. The initial EEG examination is significant as a predictor of drug resistance and diffuse slowing of the EEG baseline waveform, as well as persistent EEG features (no EEG changes after 12 months of treatment) showing a high risk of DRE [11].
All epilepsy patients, except for epilepsy with a very typical form, such as primary generalized epilepsy or Childhood benign Focal Epilepsy with a typical clinical and EEG picture that has a good response to AEDSs, should get a Magnetic Resonance Imaging (MRI) examination [12].
Diagnosis of DRE requires a correlation between neurophysiological examination and imaging of the central nervous system (CNS). In epilepsy, imaging technology can provide etiologic information regarding structural abnormalities, including potential seizure foci and functional abnormalities (such as metabolic abnormalities or blood flow or both abnormalities). [13] Abnormalities of CNS imaging examination have good predictive value in cases of DRE. [14] Different facts were found regarding the significant sensitivity between CT and MRI in diagnosing various etiological factors of DRE. MRI examination can very well detect structural lesions, such as the etiology of epilepsy. Correlation between MRI examination results and EEG examination results is essential to establish a diagnosis, determine the location of the epileptogenic focus more specifically, determine appropriate therapy, and predict the possible prognosis as DRE. [15, 16] MRI examination is rather sensitive for cases of focal epilepsy. One study in South Korea on 257 children with focal epilepsy with negative initial MRI examination results found that 79% of them were truly negative on re-MRI examination and 21% were false negatives. This can happen depending on the quality of the MRI equipment used and the implementation of special MRI examination protocols for epilepsy [15].
In Indonesia, there have been no reports on the incidence of focal epilepsy or generalized epilepsy nationally. Epilepsy data for 2018-2022 in the Pediatric Neurology outpatient at Dr. Hasan Sadikin (RSHS) hospital, Bandung, which has not yet been published, obtained 1461 cases of epilepsy, including 909 cases of focal epilepsy (62.3%) with or without drug resistance.
Based on the above background, this research was carried out to strengthen the evidence of previous research that focal epilepsy in children with structural abnormalities and the findings from EEG recordings in the form of basic wave slowing and epileptiform wave frequency consistently have good predictive value for the incidence of DRFE. This study also looked for a relationship between the results of EEG recordings and structural abnormalities from MRI examinations with DRFE. It is expected that the results of this study, with good epilepsy management guidelines accompanied by the two available modalities (EEG and MRI), can predict the risk of DRFE events. It is also expected that from this result, clinicians can plan more comprehensive management, which will also serve as important material for educating parents regarding treatment that will be faced and the possible outcomes.
2. METHODS
This quantitative comparative analysis study was carried out at Dr. Hasan Sadikin Hospital Bandung from 2018-2022. Data collection was carried out retrospectively using secondary data sources from medical records. The inclusion criteria for this study were patients with focal epilepsy in children with two or more AEDs with controlled seizures and uncontrolled seizures with at least longer than 12 months of treatment, accompanied by complete data from EEG recordings and MRI examination results. The exclusion criteria for this study were the incomplete data recorded in the medical record. Group A was pediatric patients with drug-resistant focal epilepsy, while group B was pediatric patients with drug-responsive focal epilepsy. After sample calculation using the statistical formula for comparative research using OR from previous research, the minimum total sample in each group was 32 children.
This study obtained subject data from medical records of pediatric neurology outpatients at Dr. Hasan Sadikin Hospital Bandung. The diagnosis of DRFE was clinically confirmed, and the type of seizure was determined by assessing seizure semiology based on ILAE 2017 with the supervision of a Child Neurology consultant. The results of the EEG recording accompanied the results of the EEG recording and MRI examination. The results of the EEG recording were interpreted by a pediatric neurology consultant, and a neurology radiology consultant interpreted the MRI examination results.
After obtaining permission from the ethics committee and from the head of the medical records installation, researchers collected research subjects from Child Neurology outpatients at RSHS from January 2018 to December 2023 or until the minimum sample size was met, which met the inclusion criteria and did not include the exclusion criteria.
Data collection from medical records was carried out, including:
- Patient identification includes name, gender, date of birth, onset of seizures, history of status epilepticus, history of febrile seizures, main diagnosis, comorbidities, type of regimen, and dosage of AEDs given.
- Incomplete data from medical records will be completed with parent interviews directly (during control) or indirectly (telephone interviews)
- EEG recording results from medical records and recorded data stored in the EEG computer in the EEG examination room
- Brain MRI examination results from medical records (Picture Archiving and Communication System; PACS)
All data obtained was then evaluated under the supervision of a Pediatric Neurology consultant. The type of epilepsy based on ILAE 2017 seizure semiology, findings from EEG recording results and MRI examination results, then divided into two groups: drug-resistant focal epilepsy (DRFE) and drug-controlled focal epilepsy or drug-sensitive focal epilepsy (DSFE).
The collected data will then be processed and analyzed descriptively and analytically. The descriptive of categorical data was by presenting numbers and percentages, while analytics was carried out using the Chi-square test of categorical data, specifically in connecting independent variables with related variables, presenting odds ratios, confidence levels, and a p-value <0.05, which was declared significant and carrying out multivariate analysis using logistic regression using the SPSS 25.0 application. This paper has been written according to the STROBE checklist.
3. RESULTS
Research was carried out by collecting data according to the variables to be studied. Throughout the data collection, a total of 89 subjects were included in the study, of which 22 children were excluded from the total of 89 subjects with details that one subject died, 21 subjects did not have complete data, and some had a final diagnosis of the typical epilepsy syndrome. Therefore, 67 children were obtained as research subjects, divided into 34 subjects for group A (drug-resistant focal epilepsy; DRFE) and 33 subjects for group B (drug-sensitive focal epilepsy; DSFE), as described in Fig. (1).
Table 1 summarizes the sample characteristics in this study using the chi-square test for both groups. No significantly different characteristics were found in the two groups. However, certain groups had higher percentages, such as the onset of seizures under one year being more common in group A, and the type of focal motor epilepsy was dominant in both groups. The use of anti-epileptic drugs, Valproic acid, was dominant in both groups.
There were more comorbidities in the control group than in the case group, and the differences were significant, as shown in Table 2.
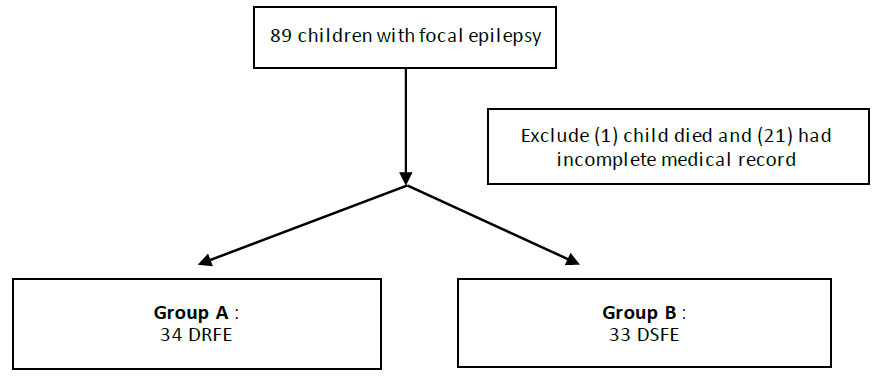
Sampling collection pathway.
Different tests were carried out on the EEG images in the two groups, which are summarized in Table 3 below. The most common features found on DRFO that were significantly different were deceleration, polyspike, and frequency >1/60s. The location of the epileptiform waves from the EEG recording results did not show significant differences in the two groups. In DRFO cases, the location of epileptiform waves was found to be most multifocal, followed by temporal and frontal.
| - | Type of Epilepsy | - | |
|---|---|---|---|
| - | - | ||
| - | DRFE | DSFE | p-value* |
| Characteristics | (n = 34) | (n = 33) | - |
| Gender : | - | - | 0,729 |
| Male | 22 (64,7) | 20 (60,6) | - |
| Female | 12 (35,3) | 13 (39,4) | - |
| Age of onset : | - | - | 0,271 |
| < 1 y.o | 19 (55,9) | 14 (42,4) | - |
| ≥ 1 y.o | 15 (44,1) | 19 (57,6) | - |
| History of status epilepticus : | - | - | 0,259** |
| Yes | 6 (17,6) | 2 (6,1) | - |
| No | 28 (82,4) | 31 (93,9) | - |
| History of febrile seizure : | - | - | 0.959 |
| Yes | 5 (14,7) | 5 (15,2) | - |
| No | 29 (85,3) | 28 (84,8) | - |
| Type of focal epilepsy : | - | - | 0,690 |
| Motor | 19 (55,9) | 16 (48,5) | - |
| Non-motor | 3 (8,8) | 5 (15,2) | - |
| Focal to bilateral | 12 (35,3) | 12 (36,4) | - |
| Type of drug : | - | - | - |
| Valproic acid | 25 (73,5) | 23 (69,7) | |
| Topiramate | 11 (32,4) | 0 | |
| Clonazepam | 3 (8,8) | 0 | |
| Clobazam | 17 (50,0) | 0 | |
| Levetiracetam | 10 (29,4) | 0 | |
| Carbamazepine | 13 (38,2) | 11 (33,3) | |
| Phenobarbital | 1 (2,9) | 0 | |
Description: DRFE (drug-resistant focal epilepsy); DSFE (drug-sensitive focal epilepsy).
| Comorbidity | Type of Epilepsy | p-value* | OR (CI 95%) | |
|---|---|---|---|---|
| DRFE | DSFE | |||
| (n = 34) | (n = 33) | |||
| Without comorbid | 1 (2,9) | 7 (21,2) | 0,034 | 1,00 |
| CP | 18 (52,9) | 8 (24,2) | 15,75 (1,65-150,15) | |
| Intellectual disability | 13 (38,2) | 15 | 6,07 (0.66-56.03) | |
| Others | 2 (5,9) | (45,5) 3 (9,1) |
4,67 (0,30-73,39) | |
| Comorbid + | 33 (97,1) | 26 | 0,027 | 8,88 (1,03 -76,84) |
| Comorbid - | 1 (2,9) | (78,8) 7 (21,2) |
- | |
Table 3.
| EEG | Type of Epilepsy | p-value* | OR (CI 95%) | |
|---|---|---|---|---|
| DRFE | DSFE | |||
| (n = 34) | (n = 33) | |||
| Abnormal | 34 (100,0) | 23 (69,7) | <0,001 | undefined |
| Normal | 0 | 10 (30,3) | - | - |
| EEG wave | - | - | - | - |
| Slowing | 30 (88,2) | 13 (39,4) | 0,000 | 11,53 (3,28-40,49) |
| Asymmetry | 3 (4,5) | 2 (6,1) | 0,667 | 1,5 (0,23-9,60) |
| Polyspike | 9 (26,5) | 5 (15,2) | 0,024 | undefined |
| Frequency >1/60 s | 26 (76,5) | 10 (30,3) | 0,000 | 7,475 (2,524-22,141) |
| Location | - | - | - | - |
| Frontal | 4 (11,8) | 5 (15,2) | - | - |
| Centrotemporal | 0 (0) | 1 (3) | - | - |
| Temporal | 8 (23,5) | 5 (15,2) | - | - |
| Midline | 1 (2,9) | 0 (0) | - | - |
| Occipital | 1 (2,9) | 0 (0) | - | - |
| Multifocal | 13 (38,2) | 6 (18,2) | - | - |
| Frontotemporal | 3 (8,8) | 2 (6,1) | - | - |
| Parietal | 1 (2,9) | 2 (6,1) | - | - |
A different test was carried out on the MRI examination results, and no significant differences were found between normal and abnormal in the two groups. However, the percentage of abnormal MRI results was greater in the case group, and the percentage of normal MRI results was greater in the control group. The most common structural lesion found was focal cortical dysplasia, at 29.4% in the case group and 33.3% in the control group.
Table 4 above summarizes the structural lesions in the form of hippocampal sclerosis, which is the second most common cause in group A and the second most common dual pathology lesion in group B. Other lesions include calcification, vascular lesions, cerebral abscesses, encephalomalacia, leukodystrophy, Rasmussen encepha- litis, and Sturge-Weber syndrome.
| MRI | Type of Epilepsy | p-value* | OR (CI 95%) | |
|---|---|---|---|---|
| DRFE | DSFE | |||
| (n = 34) | (n = 33) | |||
| Abnormal | 31 (91,2) | 25 (75,8) | 0,089 | 3,31 (0,79-13,78) |
| Normal | 3 (8,8) | 8 (24,2) | - | - |
| Hippocampal sclerosis | 6 (17,6) | 2 (6,1) | - | - |
| Focal cortical dysplasia | 10 (29,4) | 11 (33,3) | - | - |
| Tumor/cysts | 4 (11,8) | 4 (12,1) | - | - |
| Dual pathology | 5 (14,7) | 4 (12,1) | - | - |
| Others | 7 (20,6) | 4 (12,1) | - | - |
| EEG (n = 34) |
MRI (n = 34) | |
|---|---|---|
| - | ||
| Abnormal | Normal | |
| Abnormal | 31 (91,1) | 3 (8,9) |
| Normal | 0 (0) | 0 (0) |
| Variables | Coefficient | OR | Standard Error | p-value | 95% CI |
|---|---|---|---|---|---|
| EEG | 19,601 | 325 | 12195,2 | 0,999 | 0,000-0,00 |
| (EEG)Slowing | 1,912 | 6,76 | 0,9 | 0,034* | 1,160- 39,486 |
| (EEG) Spike | 0,173 | 1,18 | 0,016 | 0,900 | 0.080 – 17,581 |
| (EEG) Location | 0,196 | 1,21 | 0,158 | 0,214 | 0,893- 1,675 |
| (EEG) Frequency <1/60 | 0,972 | 2,64 | 0,866 | 0,216 | 0,485- 14,429 |
| MRI | 2,220 | 9,20 | 1,016 | 0,029* | 1,257- 67,454 |
Table 5 above shows that statistical tests could not be carried out, so there was no relationship between brain electrical activity from EEG and the image of brain lesions from MRI in 34 case subjects because the normal results in EEG recording were 0.
The variables were then subjected to multivariate analysis using logistic regression, and the results are demonstrated in the Table 6.
Table 6 describes the multivariate analysis. A significant relationship was found between the results of the EEG examination, namely slowing and MRI, with probabilities of 1.912 and 2.220, respectively, influencing the occurrence of drug-resistant focal epilepsy.
4. DISCUSSION
In this study, clinical data, EEG recording results, and MRI examination results were collected in children with Drug-Resistant Focal Epilepsy (DRFO) and Drug-Sensitive Focal Epilepsy (DSFO). The EEG recording results in the two groups were significantly different, but the MRI examination results were the same.
Several types of seizures were found to be associated with ERO, namely tonic seizures, simple partial seizures, and early onset seizures [17]. Other previous research found that a history of seizures during infancy had a significant relationship with the condition of DRE [18]. In this study, the percentage who experienced seizures earlier (<1 year) was greater in group A (55.9%) than in group B (42.4%); however, this difference was insignificant. In contrast to one study in Egypt, seizure onset was less than two years more in cases with significant values [19].
The forms of seizures in the characteristics of this study were grouped into focal motor, non-motor, and focal to bilateral epilepsy. No significant differences were found between the different tests carried out on the two groups. In percentage terms, focal motor seizures were the most common seizure type in both groups, in contrast to previous research conducted in Egypt, where the focal to bilateral type of epilepsy was found to be relatively large, amounting to 79.7% in DRFE cases [9]. There were only a few types of non-motor seizures in both groups in this study (8 subjects), due to the difficulty in establishing a diagnosis of non-motor focal epilepsy based on seizure semiology, especially in the comorbidity of CP or DI.
There was no difference in the history of febrile seizures or history of status epilepticus in the two groups [7]. It was similar to research that has been conducted in Indonesia, where the history of febrile seizures and status epilepticus was smaller in ERO cases, and no significant differences were found [7]. The risk of developing epilepsy after a febrile seizure remains controversial. One study by Neligan et al. found that the risk of epilepsy after a febrile seizure was 2-10% [20]. The pathogenetic mechanism of the relationship between febrile seizures and epilepsy was also unclear. However, several studies emphasize the genetic relationship between febrile seizures and epilepsy, where a family history of febrile seizures and epilepsy increases the risk of febrile seizures or epilepsy in children or their offspring [21, 22]. Several other studies also show that prolonged febrile seizures or status epilepticus can cause injury to the hippocampus, resulting in a high risk of developing epilepsy [23, 24].
This study found that the number of comorbidities was significantly different, where the percentage of subjects who did not have comorbidities was greater in group B. Several studies have revealed that comorbidities that are often found in children with epilepsy include intellectual disability (17%) and cerebral palsy (13.9%) [25]. Comorbidities such as neurocognitive and behavioral disorders often occur in children with epilepsy, especially in cases where seizures are difficult to control. Although most children with epilepsy have a normal global cognitive function, the risk of impaired academic performance and impaired social behavior is higher in epilepsy cases with poor seizure control [26]. This study found that FCD was the most common structural etiology in DRFE cases; it is very likely related to FCD, which can cause epilepsy, accompanied by cognitive impairment, and is at risk as an etiology of drug resistance [27, 28].
ILAE recommendations for the use of first-line drugs in focal epilepsy are Carbamazepine, Levetiracetam, and Lamotrigine. In this study, the most widely used drug was Valproic acid, which is the first-line drug for generalized epilepsy and second-line for the treatment of focal epilepsy, followed by Carbamazepine. In this study, Topiramate, Klobazam, and Levetiracetam were more widely used in DRFE cases as second and third-line drugs due to the criteria for DRFE who had consumed two or more types of drugs [29].
Abnormal EEG was found in 85.1% of patients. In previous research, several forms of brain wave abnormalities recorded on EEG were summarized, and were also related to ERO. These features include focal abnormalities, photo paroxysmal responses, slowing of activity, and other features such as eye-closure sensitivity that extends up to 1-4 seconds [30]. In this study, the images of brain waves recorded in the form of deceleration, polyspikes, and frequencies >1/60 seconds were found to be different, had a significant relationship with the DRFO event, and had different strength values. This is similar to previous research stating that drug resistance incidence was strongly correlated with EEG abnormalities such as slowing, asymmetry, abnormal amplitude, and a large number of sharp waves (>1/60s) [17]. The location of the abnormal waves does not correlate with the occurrence of DRFO, but this location determines the clinical manifestation of seizures.
EEG recording is needed to diagnose epilepsy comprehensively, even though the diagnosis of epilepsy is a clinical assessment. EEG recording was carried out to see interictal brain wave activity. Most epilepsy patients have abnormal brain activity (epileptiform waves), but they may also have a normal EEG picture. This study found no normal EEG in group A; in group B, a normal EEG was found at 30.3%. Similar to previous studies, the EEG was normal in 15.6% of cases and 26.6% of controls. 7 EEG abnormalities can be found in 2-4% of children who have never had seizures; conversely, the first interictal EEG may be normal in 55% of children with an unprovoked first seizure. EEG images alone, without regard to clinical information, cannot exclude or confirm the diagnosis of epilepsy [31].
After a multivariate analysis, it was found that two significant factors influenced drug-resistant focal epilepsy: slowing in the EEG examination and abnormalities in the MRI. If there is a slowdown in the EEG examination, the probability of resistance occurring is 1.912 times the normal population. Meanwhile, if abnormalities are found on an MRI examination, the probability of resistance occurring is 2.22 times the normal population.
This study found that normal MRI images were more common in group B than in the case group, with a significant value. There was no correlation between abnormal MRI images and the occurrence of EFRO, and no specific MRI abnormality correlated with the occurrence of EFRO. Abnormal brain lesions in the form of FCD were the most common lesions found in both groups. In contrast to several previous studies, hippocampal sclerosis was found to be the most common structural lesion in cases of drug resistance [9, 16]. Apart from FCD, this study found that hippocampal sclerosis was the second most common structural abnormality in the case group, and dual pathology was the second most common structural abnormality in group B. Hippocampal sclerosis can be accompanied by other pathologies, known as dual pathology, including neoplasms, heterotopia, ischemia, vascular lesions, brain atrophy, cysts, and other pathologies both in the temporal lobe and other brain areas [2].
There were no significant differences between MRI and EEG results in drug-resistant epilepsy in previous studies [16]. In this study, the relationship between EEG results and MRI results in group A (drug-resistant focal epilepsy) cannot be measured statistically because the EEG value was constant (normal EEG in group A is 0. Both MRI and EEG have their values for DRFE predictions [15, 17].
5. LIMITATIONS
This retrospective research requires knowledge of epilepsy semiology and collaboration with parents regarding the child's past condition as information on seizure onset so that subject data allows for bias regarding past conditions.
Additionally, MRI examinations are not routine examinations for all focal seizure conditions. Their implementation requires a long waiting time to be examined, so collecting more MRI data takes longer.
Non-motor seizure types are often challenging to recognize as the onset of seizures, not to mention in epilepsy with comorbid intellectual disability with or without cerebral palsy; direct interviews (auto-anamnesis) with patients regarding non-motor seizure types were difficult to carry out.
The onset of febrile seizures as a risk factor for epilepsy could not be determined because there was no data on the onset of febrile seizures at an early age (<1 year). The medical records only include a history of previous febrile seizures without including the age of the first febrile seizure.
CONCLUSION
There is a relationship between EEG and DRFO recording results, especially in the form of slowing of basic waves, polyspikes, and frequencies >1/60 seconds. There were more normal MRI images of DSFO than DRFO, but there was no significant difference between normal and abnormal MRI examination results in the two groups. No significant structural abnormalities were found in the DRFO cases. There was no correlation between the MRI examination results and the EEG recording results in the DRFO case. Each has a different value when predicting DRFO.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DSFO | = Drug-sensitive Focal Epilepsy |
| DRE | = Drug-Resistant Epilepsy |
| DRFE | = Drug-resistant Focal Epilepsy |
| CNS | = Central Nervous System |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the ethical commission of RSUP Dr Hasan Sadikin Bandung, with the number of approval LB.02.01/X.6.5/147/2023, Indonesia.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The selection of participants in this research took into account the voluntary principle. Participants' parents have the right to obtain an explanation of the procedures, advantages, disadvantages, and confidentiality of research data. Participants' parents' consent was obtained by signing an informed consent form.


