All published articles of this journal are available on ScienceDirect.
Snake Eye Appearance; A Rare Radiology Presentation in Acute Flaccid Paralysis: A Case Report
Abstract
Background:
Acute flaccid paralysis (AFP) is defined by the acute onset of weakness or paralysis with reduced muscle tone in children. There are many non-infectious and infectious causes. Snake eye appearance (SEA) is a rare radiologic appearance and helps narrow down differential diagnoses in flaccid paralysis.
Case Presentation:
Here, we reported a 6 months-old girl who was admitted with sudden onset flaccid paralysis. She was lethargic and ill without any detectable deep tendon reflexes. She had a high fever that had started 3 days earlier with malaise, poor feeding and coryza. The first child of the family was a boy who expired with similar symptoms; however, the reason is still unknown. Her parents were relatives (cousins). The laboratory and cerebrospinal fluid tests analysis were normal. The brain MRI analysis revealed T1 dim Hypo intensity and T2 hyperintensity along with obvious ADC map hyperintensity in the brain stem. At first, the PCR tests analysis of stool samples for poliovirus and enterovirus were normal. Spinal MRI showed snake eye appearance and helped us narrow our differential diagnosis. We repeated the PCR tests of stool because of snake eye appearance in cervical MRI that was positive for poliovirus and indicated vaccine-associated Paralytic Poliomyelitis (VAPP). Unfortunately, she expired from vaccine associated poliomyelitis.
Conclusion:
Snake eye appearance is a rare radiologic appearance that can be seen in several pathological conditions; however, it is very rare in patients with acute flaccid paralysis. Radiology signs, especially in spinal cord MRI, can help recognizing abnormalities in images, and narrow the list of differential diagnosis in acute flaccid paralysis. Therefore, spinal cord MRI has an important role in the evaluation of patient with brain stem involvement in acute flaccid paralysis.
1. INTRODUCTION
Acute flaccid paralysis (AFP) is a serious neurological illness caused by many non-infectious and infectious etiology [1]. Poliomyelitis caused by poliovirus is one of the most common infectious causes of AFP, which primarily involves children less than 5 years [2]. This clinical syndrome is characterized by the rapid weakness or paralysis of extremities, weakness of respiratory muscles and swallowing, which will be worse within several days to weeks [3]. The incidence of AFP in children under 15 years is one per 100000 cases [4]; however, this ratio is relatively higher [two per 100000 cases] in Iran because it is near polio-endemic countries such as Iraq, Pakistan and Afghanistan [5]. AFP investigation in children aged less than 15 years is usually used as a quality of syndromic surveillance. As AFP surveillance is very important step for the monitoring of the disease progress and polio eradication, the surveillance system was provided to ascertain poliomyelitis in suspected cases [6]. Additionally, laboratory investigations are performed to track or rule out the diagnosis of poliomyelitis [7].
Snake-eyes appearance (SEA) is a unique and rare radiologic finding which is diagnosed with a symmetrical and bilateral round high signal intensity lesion on axial T2-weighted MR images [8]. The radiologic appearance name came from its resemblance to the face of the snake. Several studies reported its occurrence in different conditions such as myelopathic and Hirayama diseases; however, its patho- physiological features are unclear [9]. The presence of SEA in acute flaccid paralysis is uncommon. Here, we reported a patient with Snake eye appearance on cervical spinal cord MRI who was admitted with acute flaccid paralysis.
2. CASE PRESENTATION
A six-months-old girl with a complete history of immunization was admitted to Rasool Akram Hospital (Tehran, Iran) with sudden onset flaccid paralysis and loss of consciousness. She had a high fever that had started 3 days earlier with malaise, poor feeding and coryza. Travel history was negative. There was no history of contacts with sick individuals, insect bite, toxin exposure, animal exposure, trauma and rash. She had received four doses of oral poliovirus vaccine according to the schedule recommended in Iran. According to family history, the first child of the family was boy who expired with similar symptoms mentioned above; however, the reason is still unknown. Her parents were relatives (cousins). The patient did not have any past medical problems and her growth and development were normal.
On physical examination, she was ill and lethargic. She had a blood pressure of 100 over 60, heart rate of 124/min, respiratory rate of 22/min, body temperature of 38.5oC and oxygen saturation of 98%. She was hypotonic and had areflexia. She also had pinpoint pupils but reactive to light, decreased Deep Tendon Reflexes (DTRs) and positive Gag reflex. Cranial nerve and other neurologic examinations were difficult to be assessed. There was no significant sign of respiratory, cardiovascular or skin problems.
Intravenous Vancomycin and Ceftriaxone were started. The brain CT scan revealed normal results (Fig. 1). Results from a complete blood count (CBC) were normal. Serum electrolytes, coagulation factors, liver specific enzymes, C-reactive protein, erythrocyte sedimentation rate (ESR), Creatine phosphokinase (CPK), lactate dehydrogenase (LDH), arterial blood gas (ABG), and Chest X-ray did not show any abnormalities. Cerebrospinal fluid (CSF) examination showed red blood cells (RBC) 20 per mm3 with normal glucose and protein without pleocytosis. Stool samples were examined for the possibility of Polio virus, Enterovirus and botulinum toxin and revealed negative results. By approaching Guillain-Barre Syndrome, intravenous immunoglobulin (IVIG) was started and then EMG-NCV was performed that was normal. Because of pinpoint pupils, Naloxone was administered and urine toxicology was also performed that had negative results. Intravenous Acyclovir was started because of the possibility of Brain stem encephalitis. CSF evaluation revealed negative results for the possibility of herpes simplex viruses (HSV) by PCR method and autoimmune encephalitis by measuring autoimmune antibodies. Also, GQ1b antibody checked in CSF was negative.
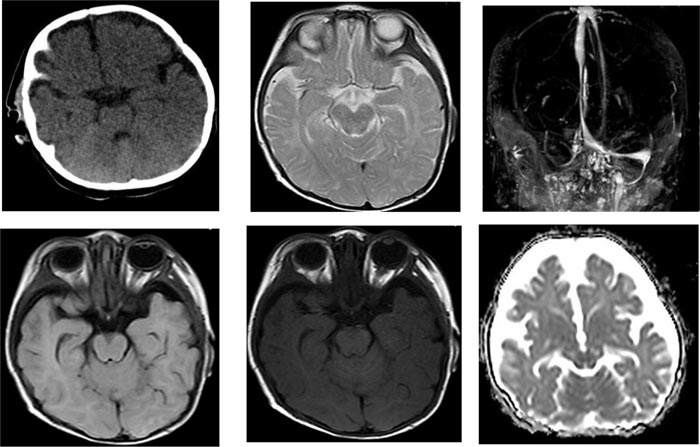
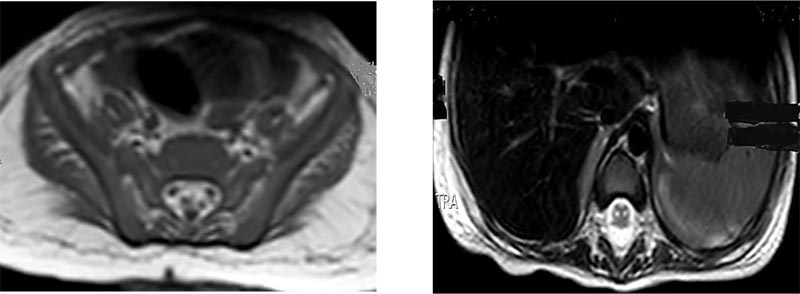
The second CSF analysis illustrated normal lactate but increased protein concentration. Brain MRI was performed and revealed T1 dim Hypo intensity and T2 hyperintensity along with obvious ADC map hyperintensity in the brain stem that is suggestive of brain stem encephalitis (Fig. 1). Brain Magnetic Resonance Venography (MRV) revealed normal results with right transvers sinus hypoplasia (Fig. 1). Because of complete paralysis of extremities and absence of deep tendon reflexes, spinal MRI was performed and revealed snake eye appearance with anterior horn cell involvement (Fig. 2). According to the result of cervical spinal MRI, stool exam was provided again to rule out the possibility of poliovirus and Enterovirus infections. The PCR test result of the second stool exam was positive for poliovirus and indicated vaccine-associated Paralytic Polio- myelitis (VAPP). The diagnosis of the patient was vaccine-associated paralytic poliomyelitis (VAPP) with probably underlying immune deficiency. Flow-cytometry analysis revealed the possibility of severe combined immunodeficiency (SCID), but her parents did not give consent for genetic evaluation. Unfortunately, the patient expired after one month of hospitalization at the pediatric intensive care unit (PICU).
3. DISCUSSION
Acute flaccid paralysis, defined by the World Health Organization (WHO), is a sudden onset of weakness and floppiness in any part of the body in a child less than 15 years age or if a physician suspects polio in any person of any age (excluding spastic paralysis, adults, cases with obvious causes like trauma or old cases) [10]. Since the eradication of wild-type poliovirus has occurred in most areas by successful vaccination programs, acute flaccid paralysis has become rare [11]. Currently, wild-type polio-virus is only endemic in Pakistan, Nigeria and Afghanistan. There have been reported cases of transmission to other countries that previously were polio-free [12]. Vaccine-associated Paralytic Poliomyelitis (VAPP) can occur with oral [Live] poliovirus vaccine [13]. In Iran, we now used oral polio vaccine.
The differential diagnosis for acute flaccid paralysis in a child can include both upper and lower motor neuron pathologies as both may present acutely with flaccid paralysis [14]. Upper motor neuron causes of AFP include postictal paresis, stroke, spinal cord pathologies related to abscess, paraneoplastic/tumor syndrome, trauma or inflammatory processes such as transverse myelitis [14]. Lower motor neuron causes include diseases that affect the muscle, neuromuscular junction, peripheral nerve and anterior horn cells. Lower motor neuron disorders that cause AFP include infections [bacterial or viral], post-infectious autoimmune conditions [for example, Guillain-Barre syndromes, brachial plexus injury/trauma, toxins [for example botulinum], and neoplasms [13]. The potential viral causes of motor neuron disease include poliovirus, non-polio enterovirus, Flavivirus (for example, West Nile virus, tick borne encephalitis), HSV, and rabies. Other causes include Borrelia burgdorferi, Corynebacterium diphtheria, Clostridium botulinum, and mycoplasma pneu- monia [15].
Here, we reported a 6 months-old girl presented with sudden onset flaccid paralysis and loss of consciousness. After several examinations and brain imaging T1 dim Hypo intensity and T2 hyperintensity along with obvious ADC map hyperintensity in the brain stem was observed. At first, the PCR tests analysis of stool samples for poliovirus and enterovirus were normal. Spinal MRI showed snake eye appearance (Fig. 2) and helped us narrow our differential diagnosis. We repeated the PCR tests of stool because of snake eye appearance in cervical MRI that was positive for poliovirus and indicated vaccine-associated Paralytic Poliomyelitis (VAPP). The diagnosis of the patient was vaccine-associated paralytic poliomyelitis (VAPP) with probably underlying immune deficiency. Flow-cytometry analysis revealed the possibility of severe combined immunodeficiency (SCID), but her parents did not give consent for genetic evaluation. Unfortunately, the patient expired after one month of hospitalization at the pediatric intensive care unit (PICU).
Snake-eye appearance has been described in association with a few lower motor neuron syndromes that include fibrocartilaginous emboli into anterior spinal artery, spinal cord infarction, poliomyelitis, resolving cord contusion due to gliosis, spondylotic myelopathy (bulging disc causing mechanical compression over radicular artery leading to chronic ischemia and gliosis in the region of anterior horn cells), brachial monomeric amyotrophy and radiation myelopathy [8]. Snake-eye appearance (SEA) was found to be due to cystic necrosis resulting from venous infarction and mechanical compression. Destruction of the gray matter accompanying significant neuronal loss in the anterior horn suggested that SEA is an unfavorable prognostic factor for the upper-extremity movements [9]. OPV vaccine [oral poliovirus vaccines] is very effective against the wild poliovirus, but in very rare cases, the vaccine can lead to paralysis. The first type of polio caused by OPV vaccine is called Vaccine Associated Paralytic Poliomyelitis (VAPP). The second form of vaccine associated polio is the Circulating Vaccine Derived Poliovirus (cVDPV). These are mutated kinds of OPV that can cause paralysis and spread from one person-to-another people. Approximately all cVDPV revolts in recent years have been caused by type 2 vaccine-derived virus. Inactivated Polio Vaccine (IPV) is a very safe vaccine in humans, whether used alone or in combination with other vaccines. No significant adverse effects have been reported, only minor side effects. IPV does not cause VAPP or cVDPV. Minor local reactions, such as tenderness and redness, may occur after IPV. IPV can be safely administered to children with immunodeficiency. Because of the increased risk of VAPP after OPV in patients with immunodeficiency, IPV is generally recommended in these children.
CONCLUSION
Snake eye appearance is a rare radiologic appearance that can be seen in several pathological conditions; however, it is very rare in patients with acute flaccid paralysis. Radiology signs, especially in spinal cord MRI, can help to recognize abnormalities in images, and narrow the list of differential diagnosis in acute flaccid paralysis. Therefore, spinal cord MRI has an important role in the evaluation of patient with brain stem involvement in acute flaccid paralysis.
LIST OF ABBREVIATIONS
| AFP | = Acute Flaccid Paralysis |
| SEA | = Snake Eye Appearance |
| MRI | = Magnetic Resonance Imaging |
| ADC | = Apparent Diffusion Coefficient |
| PCR | = Polymerase Chain Reaction |
| VAPP | = Vaccine-associated Paralytic Poliomyelitis |
| DTRs | = Deep Tendon Reflexes |
| CT | = Computed Tomography |
| CBC | = Complete Blood Count |
| ESR | = Erythrocyte Sedimentation Rate |
| CPK | = Creatine Phosphokinase |
| LDH | = Lactate Dehydrogenase |
| ABG | = Arterial Blood Gas |
| CSF | = Cerebrospinal Fluid |
| RBC | = Red Blood Cells |
| IVIG | = Intravenous Immunoglobulin |
| EMG | = Electromyography |
| NCV | = Nerve Conduction Velocity |
| HSV | = Herpes Simplex Viruses |
| MRV | = Magnetic Resonance Venography |
| SCID | = Severe Combined Immunodeficiency |
| PICU | = Pediatric Intensive Care Unit |
| WHO | = World Health Organization |
| OPV | = Oral Polio Virus |
| cVDPV | = Circulating Vaccine Derived Polio Virus |
| IPV | = Inactivated Polio Vaccine |
AUTHORS' CONTRIBUTIONS
VM, SR and PN analyzed and interpreted the patient data regarding the neurologic disease. RA and GS performed follow up the patient and were major contributors in writing the manuscript. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This case study was accredited by the Ethical Committee of Iran University of Medical Sciences.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the parents of the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
STANDARD OF REPORTING
CARE guidelines and methodology has been followed.
FUNDING
This case presentation received no specific grant from any funding agency in the public, institutions or not-for-profit sectors.
CONFLICTS OF INTEREST
The authors declare no conflict of interest in preparing this case presentation.
ACKNOWLEDGEMENTS
Declared none.


