All published articles of this journal are available on ScienceDirect.
Neurological Manifestations Associated with Synthetic Cannabinoid Use- A Case Series
Abstract
Background:
Synthetic Cannabinoid (SC) use has emerged as a growing public health threat in the United States. Several unexpected cases, presenting with a constellation of unrelated symptoms, but all having toxicity linked to SC use, have been reported in the last decade (2010-2019).
Methods:
We report a cluster of several independent cases where patients were admitted having different neurological manifestations. Extensive and expensive work-ups were performed. Upon further inspection, extended toxicology screens were found to be positive for SC metabolites.
Results:
It is alarming to observe that several reports highlight an increase in the varied and significant morbidity associated after SC use. Various SC compositions have been synthesized and distributed, with new molecules being generated at a staggering rate leading to unexpected manifestations.
Conclusion:
Young people are the most frequent users owing to its recreational effects, its easy accessibility, lower cost and difficulty in being detected in the urine by routine drug screens. From a hospital quality improvement perspective, efforts to characterize the presence of newly generated SC molecules and establish more accessible in-house screening methods will be a starting step in reducing the associated cost-burden. This will also minimize the unnecessary invasive procedures performed on a specific patient. From a socioeconomic viewpoint, solid and systematic crosstalk with increased recognition and reporting mechanism between the healthcare staff and public health personnel is strongly warranted to support state and federal regulatory efforts in combating this ongoing SC epidemic.
1. BACKGROUND
Synthetic Cannabinoids (SC) are a public health concern due to their adverse effects and public safety concerns [1]. To mimic the bliss effects of marijuana, SCs have been sprayed onto plant material, and this plant material has been consequently packaged and sold under the brand name “Spice” or “K2” [2]. Young people are the most frequent users, attributed due to its recreational effects, easy accessibility and difficulty in being detected in urine toxicology screens [3]. Patients admitted to the intensive care unit after SC exposure have exhibited significant organ dysfunction, neurologic and respiratory-related symptoms [4], having severe to fatal intoxications [5, 6]. We present a series of several independent cases where patients presented with neurological manifestations also had an array of unrelated signs and symptoms. Upon further differential and subsequent expanded toxicology screens, they were found to be positive for SC use.
2. CASE SERIES
Case 1: A 21-year-old African-American male with no remarkable past medical history was transferred from an outside hospital for continuous electroencephalogram (EEG) monitoring, after having status epilepticus. As reported by outside hospital records, the patient was out with friends at a restaurant where he acted strangely and started barking like a dog. Soon after, he became agitated, combative and difficult to control. In the emergency department (ED), he experienced generalized tonic-clonic seizures (GTCSs) for a prolonged period of time. He was therefore intubated, sedated and was given ketamine, versed and propofol. Extensive labs and magnetic resonance imaging (MRI) scans were unremarkable. EEG showed generalized slowing without active seizure or epileptiform activity. Further extensive lab testing for SC metabolites using high-performance liquid chromatography/tandem mass spectrometry (HPLC-MS/MS) revealed after two weeks that he was positive for MDMB-FUBINACA 3,3 dimethyl-butanoic acid. He was weaned off the ventilator support and extubated the next day. Upon further inquiry, the patient admitted to the use of marijuana that he exchanged with his friends, saying that it tasted funny. He did not experience further seizures (no anti-seizure drugs (ASD) were given) and was discharged with outpatient follow-ups.
Case 2: A 53-year-old African-American female with a past medical history of systemic lupus erythematosus, hypertension, hyperlipidemia, ischemic stroke, renal failure and coronary artery disease presented to the hospital with gradual loss of vision in the right eye in the last two days. Physical examination was remarkable for the lateral deviation of the right eye. Further evaluation revealed the right central retinal artery occlusion. Brain imaging demonstrated an acute right middle cerebral artery (MCA) stroke. The urine toxicology screen was negative for marijuana. The patient’s sister later reported that she used spice. Further extensive lab testing for SC metabolites using HPLC-MS/MS revealed after two weeks that she was positive for 4F1-MDMB-Butinaca. She was treated with intravenous heparin and was later transitioned to warfarin and discharged in stable condition.
Case 3: A 25-year-old African-American male with a past medical history of substance abuse had multiple admissions to the hospital for GTCS and behavioral abnormalities (walking naked and rambling). One of the episodes was reported by a bystander who indicated that he was using some sort of a smoking device. He had multiple brain MRIs, EEGs, computerized tomographies (CTs, cranial), and urine drug screens, all of which were unremarkable each time. He was on three ASDs. A subsequent lab testing for SC metabolites using HPLC-MS/MS revealed after two weeks that he was positive for 5 Fluoro ADB Carboylate. In addition, his creatinine and trans-aminase enzyme levels were elevated. The patient was referred to drug abuse rehabilitation. ASD was weaned starting from levetiracetam due to behavioral side effects and he was asked to follow-up with his neurologist. The patient was not known to have any further hospitalization since then.
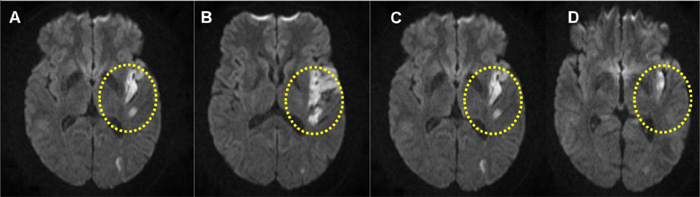
Case 4: A 46-year-old African-American male with a past medical history of hypertension was found by the bus stop in a confused state. Upon arrival to the ED, he was confused, mute with right hemiplegia and forced eye deviated to the left, cranial CT was unremarkable. According to his mother, the patient was apparently normal a couple of hours ago when they ate together at a restaurant. She also reported that he used spice, which the patient later admitted. The patient was treated according to the standard stroke protocol with intravenous tPA (tissue plasminogen activator) therapy. MRI of the brain illustrated left MCA stroke (Fig. 1). Routine urine toxicology screens showed negative results. While the mother reported intake of spice, the lab testing for SC metabolites was not performed. The patient’s weakness and speech gradually improved. He was counseled for substance abuse and discharged to acute rehabilitation.
Case 5: A-26 year-old Caucasian female, 23 weeks pregnant, came to the hospital for detox from SC use. This was the second admission within a six week period, for the same reason. The patient reported seizures associated with spice use and withdrawal. The last SC use was the day prior to admission. The patient had seizures the day after admission and the EEG showed normal awake with no seizure or epileptiform activity, whereas a previous MRI was unremarkable. A routine urine screen was negative but was positive only for cannabinoid use, six weeks earlier. Addiction medicine followed up with the patient during her admission. After a few days, she was cleared for discharge and was recommended for an outpatient follow-up with psychiatry. The subsequent lab testing for SC metabolites using HPLC-MS/MS was negative despite confirmed SC use from the patient.
2.1. Potential Cases with a Strong Likelihood of SC Toxicity
Case 6: A 29-year-old Caucasian male with a history of seizures came to the ED after having a cardiac arrest with reported asystole. Upon ED arrival, the patient was intubated and found to have elevated troponin and transaminase. The electrocardiography showed a sinus rhythm. The EEG showed marked suppression and periodic right hemisphere epileptiform discharges, hence the cardiology consultation believed that his cardiac arrest was secondary to seizures given the fact that his routine urine toxicology screens showed negative results. The cranial CT revealed anoxic brain injury and transtentorial herniation leading to acute hydrocephalus and diffuse cerebral edema. The patient developed multiple organ failure secondary to the cardiac arrest due to which the family decided to withdraw care and requested for an autopsy. The cause of death was initially attributed to his seizures, but later the autopsy revealed complications of cardiovascular cause due to vasospasm that was compounded by effects of drug use. While the expanded blood and urine toxicology screens after autopsy were positive for Δ9-tetrahydrocannabinol (THC/carboxy-THC) and indicative of marijuana use, a confirmed presence of SC metabolites remained inconclusive due to lack of performing an HPLC-MS/MS.
Case 7: A 35-year-old Caucasian male with a past medical history of hypertension, psychiatric problems and drug use (on suboxone) presented with acute left-side weakness was found to have an ischemic stroke. His hypercoagulation work-up was unremarkable. His CT angiogram (cranial) showed right middle cerebral artery severe stenosis. The rest of the stroke work-up was also unremarkable. Interestingly, his urine drug screen was negative, except for cannabinoid and carboxy-THC toxicity, which was positive. Based on his past history of drug use, together with the unclear stroke, etiology strongly suggested potential SC use. His follow-up with the stroke clinic was stable.
Case 8: A 28-year-old Caucasian female with a past medical history of seizure was admitted to the psychiatric ward for having suicidal tendencies, paranoia, violence and altered mentation. She had no history of psychiatric illnesses in the past. An extensive work-up was done to evaluate the patient, including limbic encephalitis, MRI brain (with and without contrast), EEG, autoimmune work-up, paraneoplastic panel and cerebrospinal fluid assessment to determine infection/ inflammation, all of which were found to be unremarkable. While expanded toxicology screens were not performed to confirm the detection of SC metabolites, the urine toxicology screen was positive for cannabinoid and carboxy-THC toxicity, indicative of marijuana/potential SC use. The patient gradually improved, and was discharged with a neurology and psychiatry follow-up.
Case 9: A 29-year-old Caucasian male with a past history of intravenous drug use and hepatitis C came to the ED with ongoing headache, impaired cognitive abilities, mild memory loss and blurry vision that he had for the last three months. He had some nuchal rigidity and photophobia on physical examination. The cranial MRI and CT were consistent with triventricular hydrocephalus with possible aqueductal stenosis. The patient had multiple lumbar punctures (LP) to relieve the pressure and to assess for the cause. Two LPs were positive for Candida albicans. The patient left the floor multiple times to smoke and when he got back reported having an exacerbation of his symptoms. The routine urine drug screen performed each time upon his return was found to be negative. An electronic cigarette and unknown brown substance (resembling SC) were also found in his room. Expanded toxicology screens were not performed to confirm the detection of SC metabolites. The patient was prevented to further leave the hospital bed to smoke. He and his visitor were monitored closely. He continued to improve and was discharged in a stable condition.
3. DISCUSSION
Cannabis is increasingly present in our society, both for its recreational and medical use [7]. SCs, initially developed as pharmacological tools to probe into the endocannabinoid system and for its use as novel pharmacotherapies, are now highly abused [8]. First introduced as recreational drugs [synthetic marijuana] in Europe in 2006, its consumption has increased in the USA since 2009 [9]. This is a serious public health and social problem throughout the world as it is highly challenging to identify which SC was consumed, a necessary step to link adverse health effects to the new drug's toxicity. Our case series is unique, as it is one of the few reports that not only identify the association of neurological problems with SC toxicity, but also confirm the presence of specific SCs in some of the cases (Table 1).
Younger male SC users appear to experience more psychotic symptoms compared to those who use marijuana [10]. This result tends to resonate with what we observed with some of our patients, one of whom was periodically observed to “bark like a dog” (case 1) while another was “walking naked and rambling” (case 3). Neurophysiology studies have documented similarities between disruptions of neuronal network oscillations in schizophrenia and psychosis to those triggered by SC, identifying that there are more psychotic symptoms and agitation among SC users than in those ingesting cannabis [11]. In addition, SC use has been linked to pathophysiological states such as adverse cardiovascular events [12, 13] and impaired neurocognition [14].
3.1. Reducing Unnecessary Costs
As observed in our case series, SCs can cause or precipitate various neurological manifestations that can prompt the physicians towards ordering extensive investigations and unnecessary procedures, while critically trying to analyze various differential diagnosis such as autoimmune/limbic encephalitis. The routine tests ordered to confirm or negate diagnosis (for example, performing LP or an MRI to rule out the possibility of limbic encephalitis) are costly and time-consuming. Moreover, SC use has been observed to result in diagnosable psychotic disorders requiring more pharmacotherapy with antipsychotic medications and/or longer psychiatric hospitalizations compared to marijuana or natural cannabis use [15]. Psychosis can persist even without a history of mental illness and has been reported to develop into chronic schizophrenia.
3.2. Toxicology Screen Limitations
So far, two cannabinoid receptors (CB1R and CB2R) have been cloned and characterized [2]. The SCs have been shown to maintain their affinity and functional activity for CB1R and CB2R and have been shown to cause severe harmful effects when compared to the effects of Δ9-THC. In recent years, natural preparations with user-tailored compositions and new SC with high pharmacological potency have appeared, highlighting the discrepancy in the production of natural and synthetic compounds [7]. Due to this, SC metabolite screening and confirmation assays need to be constantly updated to identify emerging SC intake. Moreover, the time and skills required to determine optimal SC marker metabolites from the highly complex HPLC-MS/MS data obtained are labor intensive and time-consuming. Rapid publication of marker metabolites and the availability of human urine specimens to verify these markers for monitoring are also required.
Two intrinsic properties complicate SC identification, their often rapid and extensive metabolism, and their generally high potency relative to the natural psychoactive THC in cannabis [8]. The analysis of SC compounds in a urine sample is currently one of the more complex tasks facing toxicologists. The list of prevalent compounds in circulation at any given time is constantly changing at a rapid rate to avoid legal control and, to a lesser extent, avoid detection [16]. Even with the knowledge of the chemical entities, their detection in urine is complicated by the fact that they are present exclusively as both phase I metabolites and phase II conjugates.
Based on what we observed in our case series, we suggest that an SC toxicology screen should be performed in those patients with unexplained neurological symptoms (Table 2) and with negative routine drug screens (for drugs such as cocaine and amphetamines). In our study, the specialized HPLC-MS/MS screens were performed only in some patients. The neurological differentials and follow-up prior to the suspected toxicity happened over a period of time. Hence, it was only later that the specialized screen (the HPLC-MS/MS) was sought after at different timelines for different patients. Many of the patients were managed successfully due to awareness generated about the drug and its symptoms, and in taking a detailed history from either the patient or family, who when specifically asked, confirmed suspicions about spice/K2 consumption (some patients even considering it as a natural/herbal drug). Some of the screening tests were inconclusive due to the constant altering of SC metabolites. For example, in case 5, the SC screen result was negative despite the patient admitting to its use. From a hospital quality control perspective, it will be ideal if SC screening becomes available in most hospitals rather than being sent out, and for it to be constantly updated as per the changing SC market. Applying such an in-house screening for suspected patients, in addition to counselling and well-being, management is likely to decrease hospital cost, unnecessary expensive testing, prescribing medications and procedures that could be potentially harmful to the patient.
Interestingly, a strategy has been developed for characterizing SC metabolism and identifying suitable marker metabolites for new SC [8]. The goal has been to rapidly publish results to enable clinical and forensic toxicology laboratories to include target metabolites into SC screening and confirmation methods, and to identify optimal targets for reference manufacturers to synthesize as analytical standards. The routine adolescent postmortem toxicology does not include an SC analysis, thus masking the true burden of fatalities related to SCs. With the synthetic drug use on the rise, forensic experts should carry a high degree of suspicion for the possibility of SC intoxication in adolescent fatalities when no other discernible cause of death has been identified [17].
3.3. Raising Awareness
Our case series sheds light on the different neurological manifestations of SC drugs. The special tests that are designed to spot these chemicals are not FDA approved or readily available making it extremely difficult to detect, partially contributing to their popularity. With insight into drug history, physicians can avoid falling into the trap and thus can decrease the cost burden of care in these patients. An effective FDA approved test can tremendously help the health care providers to promptly diagnose the patients and direct the therapy to prevent more harm.
It is important for clinicians and the treatment staff to keep abreast of the current SC drug trends and, when necessary, collaborate with pharmacists, law enforcement, toxicologists, and mental health providers in discussing and implementing strategies for addressing SCs intake and their resulting toxicities. An in-house assessment of SC toxicity and quicker availability of the results will help in reducing further unnecessary testing and procedures. From a larger perspective, to counter this growing challenge, global collaboration is critical. Agencies such as the FDA, EMCDDA, NIDA, and the new UNODC on Early Warning Advisory are promising examples of relevant efforts for rapid information sharing between global government agencies and the scientific community. Crosstalk and collaboration between forensic toxicology laboratories and legitimate suppliers of analytical standards may result in better preparation and a timelier response to future SC outbreaks. For example, a positive trend that is the recent reduction in new SC introduced per year has been observed, and this is perhaps a result of global collaboration, especially with the involvement of the Chinese government [8]. However, as governments tighten scheduling laws, it is indeed a vicious circle as more complicated or
| Cases | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| Age (years) | 21 | 53 | 25 | 46 | 26 | 29 | 35 | 28 | 29 |
| Gender (male/female) | M | F | M | M | F | M | M | F | M |
| Neurological complications | Seizure and abnormal behavior | Ischemic stroke | Seizure and abnormal behavior | Ischemic stroke | Seizure | ABI, brain herniation and edema | Ischemic stroke | Abnormal behavior, altered mental status | Meningitis, hydrocephalus |
| Routine urine screening for cannabinoids | + | - | - | - | +/- | + | + | + | - |
| SC testing (HPLC-MS/MS) | + | + | + | ND | - | ND | ND | ND | ND |
| Confirming SC use | Patient himself | Family | Bystander | Family | Patient herself | - | - | - | - |
| Death | - | - | - | - | - | + | - | - | - |
| Age |
| • In our study, more SC users were young (within their 20s-30s). Younger males generally tend to use SC more than younger females. |
|
Symptom characteristics (one or more of the below may be linked to SC toxicity) Psychiatric and neurological- |
| • Unusual/abnormal behavior (for example – barking like a dog; running naked) • Seizure/epilepsy episodes – with negative imaging or with negative regular drug screen and/or no known history/family history of seizure |
| Cardiovascular- |
| • Cardiac arrest - leading to multiple organ failure, subsequently resulting in anoxic brain injury (particularly in young patients with no known risk
factor and negative regular drug screen). • Stroke – in young patients with no risk factors or genetic predisposition and/or with negative regular drug screen |
| Declared assumption of SC drug use |
| • Patients (particularly young) with unexplained neurological symptoms and negative routine drug screens (for drugs such as cocaine and amphetamines). |
| Toxicology assays |
| • Preliminary testing using routine urine screens (while this test helps to explain if other drugs may be a cause for the associated neurological symptoms, but this test does not indicate whether a patient has truly consumed SC or not). • Confirmation for the presence of SC metabolites using urine/serum HPLC-MS/MS screen will be helpful if it comes back positive. A negative result, however, does not rule out the possibility of SC consumption. Limitations include the time taken for the screen result to come back (usually obtained in 2-3 weeks) and the need for constantly updating the list of new SC metabolites. |
| Recovery/rehabilitation |
| • The recovery varies and depends on neurological symptoms. • Most patients recover well but usually have prolonged hospitalization and multiple testing. Recovery also is strongly dependent on the type of SC metabolites that have been used. • Upon confirmation of SC toxicity, the involvement of addiction medicine and counseling early on is likely to aid in the recovery/rehabilitation process. |
uncommon SC principal moieties or secondary substructures may emerge within the market, thus highlighting the pivotal need for educating the public. The requirement for forensic toxicologists to identify optimal target metabolites for the continuously changing SCs and to evaluate new metabolic patterns is likely to continue into the near future.
CONCLUSION
SC abuse is a critical public health problem, often resulting in many ED visits and fatalities. Despite government efforts in curbing its use and categorizing it as illegal, novel SCs are consistently introduced. Major hurdles are the cost of HPLC-MS/MS for non-targeted urine SC screening, and the time and skills required to determine optimal SC marker metabolites from the highly complex HPLC-MS/MS data obtained. Clinicians should be aware of the different neurological and psychiatric manifestations of the toxicity. State-wise, national and global efforts of a highly collaborative nature are mandatory in educating the people about the severe manifestations of this drug.
AUTHORS' CONTRIBUTIONS
M.E., S.N. collected the data, analyzed the literature, and wrote the manuscript. M.E., S.N., P.B., A.H., C.S. and R.B. analyzed the literature. W.L., C.J., A.H., K.R. and A.P. reviewed and edited the manuscript. All the authors read and agreed to the final version of the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
A thorough review from the institutional review board (IRB) number 20.0137 at the University of Louisville, USA, has been performed.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used in the study that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
STANDARD FOR REPORTING
Care guidelines and methodology were followed to conduct the study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


