All published articles of this journal are available on ScienceDirect.
Brain Tumor in Differential Diagnosis of Seizures in Puerperium: Case Report
Abstract
Convulsive crisis is a transient disturbance of cerebral function, and the etiology of which may be manifold. Its clarification is essential for establishing adequate therapy and seizure control. In the pregnancy-puerperal cycle, eclampsia is the most common cause of it, but brain tumor, epilepsy and other disorders are part of the differential diagnosis. We report a case of seizure triggered by tumor in a primigest, 22 years old, at 38 weeks’ gestation with premature rupture of membranes. Cesarean section was performed due to non-reassuring fetal condition. On the second day of puerperium, she presented recurrent episodes of generalized tonic-clonic seizures and elevated blood pressure. She received magnesium sulfate for 24 hours and persisted with severe headache. Magnetic resonance imaging of the brain showed an expansive lesion in the left frontoparietal region. The patient underwent intracranial microsurgery on the eighth day after cesarean section, with complete resection of the lesion and anatomopathological diagnosis of schwannoma. She went through good postoperative evolution, without neurological deficits, and stayed on phenobarbital, with no seizures until 6 months of follow-up. From the case we conclude that although the first diagnosis in pregnant or puerperal women with seizures should be eclampsia, there are other causes, such as brain tumor and Posterior Reversible Encephalopathy Syndrome (PRES). Careful evaluation is required, especially in refractory cases and not responding to usual treatment.
1. INTRODUCTION
Neurological disorders manifested in pregnancy may be directly associated with it (pre-eclampsia, eclampsia) or may be related to preexisting conditions (epilepsy, multiple sclerosis, myasthenia gravis, brain tumor), which may be exacerbated during pregnancy and the puerperium due to physiological changes associated with this period [1]. Convulsive crisis is a transient disturbance of cerebral function. Multiple factors can be involved in the etiology of this disorder, and its clarification is essential for establishing adequate therapy and seizure control. During the pregnancy-puerperal cycle, eclampsia is the most frequent cause of the first convulsive manifestation [2]. Its incidence has declined over the years in areas with increased health care, which includes adequate prenatal care. The incidence rate reported in Latin America (0.14%) is approximately three times greater compared to the one found in the United States (range of 0.03% to 0,05%) [3, 4]. However, other causes of convulsive crisis should be investigated or excluded, especially in refractory cases that do not respond to usual treatment. Although the incidence of brain tumor does not increase during pregnancy, it may become symptomatic and voluminous due to water retention and hormonal action resulting from this period [5, 6]. This report aims to describe a patient with convulsive crisis in the puerperium triggered by brain tumor, occurred in Hospital de Clínicas de Porto Alegre (HCPA), public-private hospital linked to educational institution Federal University of Rio Grande do Sul (UFRGS).
2. CASE REPORT
A 22-year-old, primigest, caucasian, and obese (BMI: 36.3) woman was admitted at 38 weeks’ gestation due to premature rupture of membranes. On admission, normal and stable vital signs (blood pressure: 128/79 mmHg; heart rate: 80 bpm) were observed. During induction of labor with oxytocin, patient stayed assintomatic, evolving into cesarean delivery due to non-reassuring fetal condition. Patient presented convulsive crisis 26 hours after cesarean section, and laboratory test revealed urinary protein/creatinine ratio of 0.91. Patient was diagnosed with eclampsia, and received magnesium sulphate for 24 hours. She persisted with headache, and evaluation with anesthesiologist was performed due to suspicion of post-rachi headache. A new seizure was reported on the fourth day of hospitalization. The evolution of the puerperium is presented in Table 1.
| Date | Evolution | Conduct |
|---|---|---|
| 1st PO Caesarean | Patient presented with convulsive crisis. | Administration of magnesium sulphate and requested exams. |
| 3rd - 5th PO Caesarean | Persistence of headache. New convulsive crisis. | Neurology team evaluation. It was requested a brain MRI with contrast and angioresonance of intracranial veins and arteries. Initiated Phenytoin 100 mg oral. |
| 6th PO Caesarean | New convulsive crisis. | Maintenance of anticonvulsive monotherapy. |
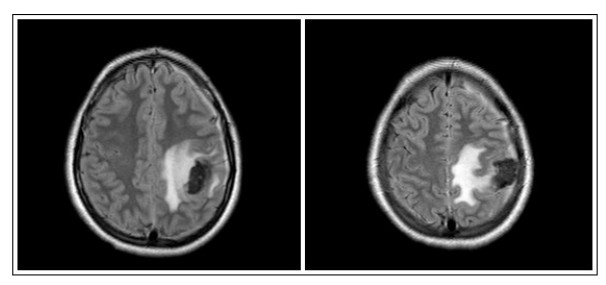
| 7th PO Caesarean | New convulsive crisis. Brain MRI reveals frontoparietal expansive lesion at left with perilesional edema, probable neoplasia (Fig. 1). | Transfer to neurosurgery team. Administration of intravenous Diazepan and Phenytoin. Surgical procedure indicated. |
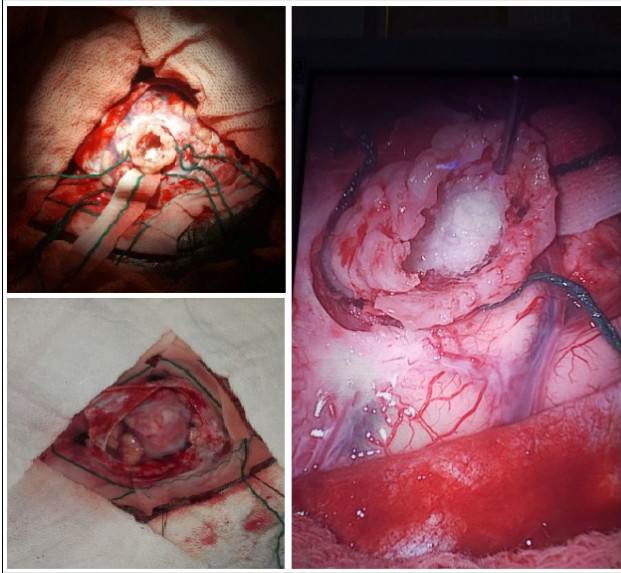
| 8th PO Caesarean | Patient undergoes neurosurgery (Fig. 2). | Complete lesion resection without intercurrences. |
| 1th - 3rd PO Intracranial Microsurgery |
Focal crisis persistence. | Alteration of anticonvulsant for Carbamazepine. |
| 6th PO Intracranial Microsurgery |
Good postoperative evolution, and good oral acceptance. No more generalized seizures. Patient is able to walk with no difficulties. | Hospital discharge. |
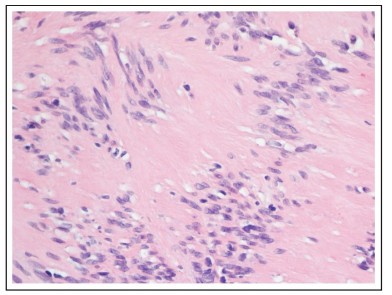
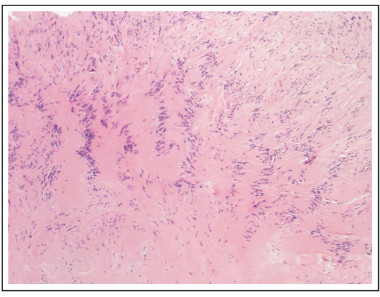
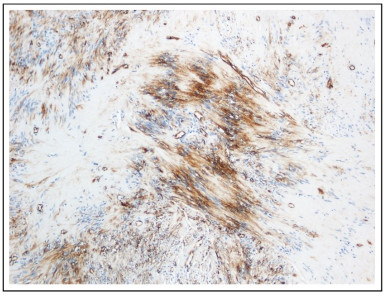
Pathology identified an encapsulated lesion composed entirely of well-differentiated Schwann cells, with eosinophilic cytoplasm, indistinct cell membranes and tapered nuclei. Areas of compact spindle cells (Antoni A) with nuclear palisading and Verocay Bodies were alternated with hypocellular less orderly areas (Antoni B) (Figs. 4 and 5). Mitoses were not observed. The blood vessels have hyalinized walls. The lesion presented SOX-10 and CD34 immunoreactivity (Fig. 6).
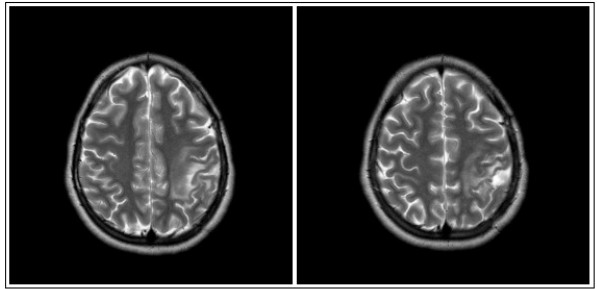
At follow-up of 6 months, patient had no neurological deficits or new generalized tonic-clonic seizures in the use of phenobarbital. Brain MRI at 8th month of follow up showed complete remission of the lesion (Fig. 3).
3. DISCUSSION
Clinical manifestation of neurological diseases is often reported during gestation and puerperium due to physiological changes observed in these periods. It is necessary to understand those conditions in order to better assist their diagnosis and treatment. For example, increasing levels of procoagulant factors and fibrinogen in contrast to decreased production of fibrinolytic agents leads to a state of hypercoagulability, which results in a greater risk of venous thromboembolism. Other changes related to renal clearance and hepatic metabolism also influence some drugs pharmacokinetics, such as anticonvu-lsants, and may lead to an increase in the number of seizures if there is no dose adjustment [1, 7].
In addition to preexisting diseases that may be exacerbated in the pregnancy-puerperal period, Eclampsia, a pathology directly related to pregnancy, is usually the first diagnosis to be considered in a pregnant or puerperal woman who presents with acute neurological symptoms [8]. A detailed anamnesis of the patient's symptoms is essential to support the diagnostic investigation.
Headache is the most common neurological symptom in pregnancy. Tension and migraine are the most frequent types among pregnant and postpartum women [8]. The patient reported in this case is among the 40% who present this symptom in the first week of puerperium [9-11]. She characterized the pain as pressure in the frontal and occipital regions, with improvement towards the decubitus and worsening towards the orthostatism. No other symptoms were reported. When headache is related to preeclampsia, it is usually throbbing, bilateral, and may be associated with scotomas, hypertension, epigastralgia, edema and proteinuria [12-14]. However, some warning signs suggest a secondary cause. Cases of abrupt headache, severe intensity, and with a different pattern from usual should be promptly investigated [15]. Causes such as acute subarachnoid hemorrhage, reversible posterior encephalopathy syndrome, cerebral venous sinus thrombosis, reversible cerebral vasoconstriction syndrome, and cervical-cranial artery dissections should be excluded by computed tomography, magnetic resonance and/or lumbar puncture. Patients who underwent spinal anesthesia (subarachnoid block or spinal anesthesia) during labor and/or cesarean section may experience headache after accidental puncture of the dura mater. It occurs between 1 and 7 days postpartum, and it is often located in the nuchal and occipital regions, with more severe pain towards orthostatism region, and improvement after 10-15 minutes of decubitus. Neurolo-gical symptoms, nausea, vomiting, and intense incapacitation may also be observed [10]. In the aforementioned case, there were no records of accidental puncture or difficulty in performing both anesthesia of labor and cesarean section. Besides, the non-classical clinical presentation makes this etiology less likely for the headache.
Women with seizures in the pregnancy-puerperal cycle can be divided into 3 categories: the first includes the majority of patients, who have established epilepsy prior to gestation; the second involves women who present their first crisis in this period, but it is not directly related to gestation and puerperium (for example, due to brain tumor or hypoglycemia), and the third group is represented by patients who also present the first crisis in this period, but as a manifestation of a pathology directly related to gestation (e.g, eclampsia, reversible posterior encephalopathy syndrome, intracranial hemorrhage, venous sinus thrombosis, among others) [8, 16].
Epilepsy is the most common chronic neurological disorder, affecting 0.7% of the population. The majority of patients remain without seizures or with no changes in the previous pattern. However, due to the metabolic and hormonal changes of this period, there may be a need for larger doses of anticonvulsants for this to occur [7]. Symptoms associated with seizures include the presence of aura, focal or generalized motor movements, changes in breathing pattern, loss of consciousness and function of the bowel and bladder. The crisis can be followed by amnesia, lethargy, headache, muscle pain and transient focal weakness [17]. The onset of epilepsy in pregnancy is less common, as its incidence peaks are in childhood and old age. Therefore, acute seizures in this period require urgent investigation [1].
It has been reported that 44% of seizures related to eclampsia occur in the puerperium, 38% prepartum and 18% intrapartum [7]. It may be preceded by symptoms such as persistent frontal or occipital headache, blurred vision, photopsia, photophobia, and altered level of consciousness lasting about 1 minute [1]. It is related to hypertension, edema and proteinuria [2]. Magnetic resonance imaging of the brain may reveal cortical and subcortical hyperintense lesions, predominantly in the posterior region, classifying the condition as Posterior Reversible Encephalopathy Syndrome (PRES) [7].
The state of hypercoagulability associated with pregnancy and puerperium contributes to an increase in the incidence of cerebral venous thrombosis in this period. Headache occurs in 95% of the patients, with about 50% of them presenting convulsions or focal neurological deficits, and papilledema or mental status changes can be observed in a third of the cases. There is also a greater occurrence of subarachnoid hemorrhage in pregnancy and puerperium due to an increase in cardiac output and to hormonal effects in the vasculature, being one of the differential diagnoses to be considered [2].
Convulsive crisis affect 50% to 80% of patients with a primary brain tumor, so one should pay attention to this diagnostic hypothesis [18]. There is no increase in its incidence during pregnancy, however, some tumors may grow and become symptomatic due to water retention and hormonal changes arising from this period [19]. Tumor-related seizures may be focal, with secondary generalization, repetitive, associated with post-ictal status, and focal neurological findings on imaging tests (preferably contrast magnetic resonance imaging) [18, 20].
Regarding the patient in our report, despite the evidence of hypertension and proteinuria from the first convulsive crisis, the persistence of the episodes despite the standard treatment for eclampsia led to the finding of the intracranial lesion in the imaging exam. After its complete removal, the patient remained without new generalized seizures or neurological deficits following a 6-month follow-up.
CONCLUSION
Although the first diagnosis in pregnant or postpartum women with seizures is usually eclampsia, there are other causes for their occurrence that should be investigated or excluded. In cases of neurological symptoms with acute onset in this period, the investigation should also cover causes not related to gestation, such as brain tumor. Careful assessment is required, individualizing the patient's clinical condition, especially in refractory cases and not responding to usual treatment.
FUNDING
None.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


