CASE REPORT
Post-COVID-19 Olfactory and Gustatory Dysfunction: Photobiomodulation Therapy as a Treatment Option in a Series of Cases
Déborah Santos Sales1, 2, *
Article Information
Identifiers and Pagination:
Year: 2023Volume: 17
E-location ID: e1874205X2309190
Publisher ID: e1874205X2309190
DOI: 10.2174/011874205X254822230922114001
Article History:
Received Date: 24/03/2023Revision Received Date: 27/07/2023
Acceptance Date: 13/08/2023
Electronic publication date: 23/10/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
Coronaviruses patients may develop various neurological complications, including loss of smell and taste. Rehabilitation programs should be considered for patients with disabilities lasting longer than two weeks. The present pilot study evaluated photobiomodulation therapy (PBMT) as a treatment option for olfactory and gustatory dysfunctions.
Case Representation:
The study included six patients with coronavirus disease with olfactory and gustatory complaints who were part of a cohort of 172 coronavirus disease patients monitored for late neurological manifestations. Olfactory and gustatory functions were evaluated using visual analog scales applied at baseline, end, and 6 months after treatment. 36-item Short-Form General Health Survey and a questionnaire containing closed questions were also administered. All scales were applied by a researcher blinded to the results of the given intervention. An intranasal PBMT protocol was applied, with 16 laser sessions performed twice a week at a 48-hour interval.
Results:
A statistically significant difference was observed between the medians of the visual analogue scale scores for olfactory and gustatory disorders before, after, and six months later. The medians of the physical role, social functioning, general health, and emotional role SF-36 domains were higher after treatment, suggesting improved quality of life.
Conclusion:
The results observed in this study suggest that PBMT can be an effective resource for patients with long-term COVID-19.
1. INTRODUCTION
Numerous researches have examined the intricate clinical profile of COVID-19 across time, including atypical symptoms relating to many physiological systems. Further, a wide range of neurological symptoms, primarily brought on by the involvement of the central nervous system (dizziness, headache, cerebrovascular diseases, meningitis, encephalitis, seizures, and ataxia), peripheral nervous system (anosmia, ageusia, visual impairment, paraesthesia, nerve pain, and Guillain-Barré syndrome), and skeletal muscles has also been reported [1].
There are an increasing number of reports of persistent and prolonged effects after the acute phase of COVID-19. The long-term COVID-19 syndrome is characterized by persistent symptoms and/or late or long-term complications beyond 4-12 weeks from the onset of symptoms [2]. Although the prevalence of olfactory and taste dysfunction has declined continuously after acute COVID-19, many patients had persistent chemosensory disorders 3 months to 2 years after symptom onset [3, 4].
The loss of smell and taste can lead to risks since the perception of odor and taste sources is a protective factor against dangers such as fire, gas, or food poisoning. Studies show that patients with prolonged loss of smell often have depressive symptoms, decreased self-esteem, loss of intensity of emotional experiences and lower overall quality of life [4-6].
The treatment for anosmia and ageusia varies and may include olfactory and gustatory training, the use of topical and systemic corticosteroids, use of carbamazepine among others [7-9]. However, to date, there is no description of a 100% effective treatment for the recovery of smell and taste in these patients. When the impairment lasts longer than 2 weeks, some therapeutic modalities should be considered [10]. Photobiomodulation therapy (PBMT) represents a new and viable therapeutic modality for the rehabilitation of taste and smell disorders for the treatment of COVID-19, as it is capable of modulating inflammatory processes and improving tissue healing in a general manner [11, 12].
Photobiomodulation (PBM) provides neuroprotection through anti-inflammatory and antioxidant pathways [12, 13]. This pilot study primarily describes the use of photobiomodulation as a possible treatment option based on the previously established mechanism of action of this therapy and its impact on the quality of life (QoL) of this patient.
2. MATERIALS AND METHODS
A total of 172 patients with COVID-19 were monitored for late neurological manifestations at a University Hospital from March to December 2021. This study included patients with the mild form of the disease and with persistent complaints of olfactory and gustatory dysfunction for at least 6 months. Patients hospitalized or using mechanical ventilation due to COVID-19 infection were excluded. COVID-19 was confirmed using a biomolecular assay (RTPCR). All patients agreed to participate in the study and signed an informed consent form. The study was approved by the local research and ethics committee (registration number CAAE:33659620.1.1001.5258).
3. QUANTIFICATION OF IMPAIRMENT OF THE OLFACTORY AND GUSTATORY FUNCTION
Olfactory and gustatory functions were evaluated separately using two visual analog scales (VAS) ranging from 0 (normal smell/taste) to 10 (complete absence of smell, anosmia, taste, and ageusia) applied at the first clinical appointment (baseline), after the end of the treatment, and 6 months later. The Medical Outcomes Study 36 - Item Short-Form Health Survey (SF-36) SF-36 were applied before and after treatment. SF-36 is a widely used scale that evaluates health-related QoL, and its reliability and validity have been documented in Portuguese. It comprises 36 questions that cover eight domains of health. Each domain was scored on a 0–100 metric scale, with a higher score reflecting better health. A mean score of 50 was considered a normative value for all subscales [14]. All scales were applied by a researcher blinded to the results of the given intervention.
A questionnaire containing closed questions related to self-perception of olfactory disorders (OD) and the frequency of identification of odors, such as smoke and gas leaks, was administered before and after the end of treatment.
4. PHOTOBIOMODULATION PROCEDURE
An intranasal PBMT protocol was applied using Laser DUO® (MM Optics Ltda São Carlos, SP, Brazil) at 660 nm in contact mode, with 100 mW of power and 8 J of energy in each nasal mucosa and 6 J at ten points on the tongue. A total of 16 laser sessions, twice a week and with a 48-hour interval, were performed.
5. STATISTICAL ANALYSIS
A paired Friedman two-way analysis of variance was used to check whether there was a significant difference between the OD and taste disorders (TD) scores before, after treatment and six months after treatment. The Wilcoxon test for related samples was used to analyze whether there was a significant difference between SF-36 domain scores before and after treatment. The mean differences in QoL at specific scales were considered clinically relevant if a minimum discrepancy of 10 points was found [15]. Statistical significance was set at p < 0.05. SPSS software (version 22.0) was used for all the analyses.
6. RESULTS
Six patients (five women and one man) were treated with PBMT because of persistent complaints of anosmia/ageusia. The median age was 42 [36.3-63.3] years, and none of the patients were older than 64 years. Patients had a median schooling time of 16.5 [12.0-24.0] years. All patients completed the protocol (16 sessions). No adverse or unanticipated events emerged. The median time to maintenance of olfactory and gustatory disorders was 13 [10.8-13.0] months. The frequency of responses related to olfactory disorders before and after PBMT is shown in Table 1. There was a statistically significant difference between the medians the visual analog scales of olfactory and gustatory disorders before the beginning of treatment, at the end of 16 sessions, and 6 months later (Table 2).
Most of the patients maintained an improvement in the functions of smell and taste 6 months after the end of the treatment, except for one patient who improved at the end of the treatment but regressed on the visual analog scale for both smell and taste functions (Fig. 1).
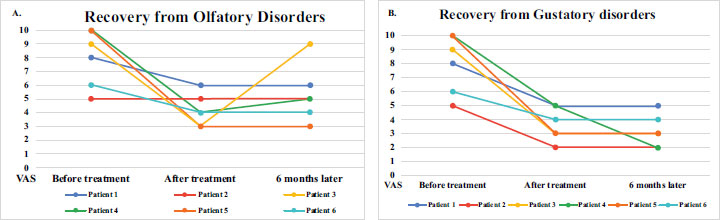 |
Fig. (1).
Recovery form olfactory (A) and gustatory (B) disorders over time evaluated using visual analog scales. Abbreviation: VAS, visual analog scales. |
| - | Photobiomodulation Therapy | |||
| - | Before Treatment | After Treatment | 6 Months Later | P-value |
| Disorders | - | - | - | - |
| Olfatory, Median [IQR] | 8.5 [5.8–10.0] | 4.0 [3.0–5.3] | 5.0 [3.8–8.0] | 0.014* |
| Gustatory, Median [IQR] | 8.5 [5.8–10.0] | 3.5 [2.8–5.0] | 3.0 [2.0–4.2] | 0.003* |
| SF-36 Quality of life Mean. SD | - | - | - | - |
| Physical function | 70.0 ± 16.7 | 72.5 ± 25.0 | Not available | 0.89 |
| Role physical | 45.8 ± 51.0 | 62.5 ± 37.9 | Not available | 0.02** |
| Body pain | 59.3 ± 28.0 | 61.8 ± 17.6 | Not available | 0.67 |
| General health | 42.1 ± 16.7 | 73.3 ± 10.3 | Not available | 0.28** |
| Vitality | 40.0 ± 33.9 | 45.8 ± 23.5 | Not available | 0.59 |
| Social functioning | 62.5 ± 29.6 | 45.8 ± 36.8 | Not available | 0.04** |
| Role emotional | 33.3 ± 51.6 | 45.7 ± 48.8 | Not available | 0.18** |
| Mental health | 55.3 ± 31.2 | 52.6 ± 30.0 | Not available | 0.75 |
| Questions | Answer Options |
Before Treatment N (%) |
After Treatment N (%) |
| How do you consider your sense of smell? | Good Reasonable Bad |
0 (0) 2 (33.3) 4 (66.7) |
2 (33.3) 4 (66.7) 0 (0) |
| How often do you smell smoke? | Ever Sometimes Never |
0 (0) 1 (16.7) 5 (83.3) |
2 (33.3) 3 (50.0) 1 (16.7) |
| How often do you smell gas leaking? | Ever Sometimes Never |
0 (0) 1 (16.7) 5 (83.3) |
3 (50.0) 0 (0) 3 (50.0) |
| How often do you smell food? | Ever Sometimes Never |
0 (0) 3 (50.0) 3 (50.0) |
2 (33.3) 3 (50.0) 1 (16.7) |
| How often do you smell perfume? | Ever Sometimes Never |
0 (0) 3 (50.0) 3 (50.0) |
2 (33.3) 3 (50.0) 1 (16.7) |
Regarding QoL, there was a statistically significant difference and clinical relevance between the medians of the role of physical, social functioning, general health, and role emotional SF-36 domains before and after treatment, which corroborates the hypothesis that the improvement of olfactory and taste sensations can directly impact both the general health and social aspects of the quality of life of individuals with long-term COVID-19 (Table 2).
7. DISCUSSION
Our series of cases with 6 patients with persistent complaints of olfactory and gustatory dysfunction for at least 6 months after a mild form of COVID-19, like these other studies, had a high prevalence of women [4, 16]. More recently, the female sex was pointed as one of the risk factors for persistent long-term olfactory and gustatory dysfunction due to COVID-19 [4]. Additionally, female gender was strongly associated with being less likely than men to recover the sense of smell [17].
The photobiomodulation has been documented in literature as immunomodulator therapy with antioxidant and anti-inflammatory effects. It is also effective in reducing inflammatory cytokines through PBM and Ca2+ cell signaling sensitivity, which explains its anti-inflammatory effects [18]. In our pilot study, the findings showed significant improvements in olfactory and gustatory functions after this therapy, but not completely. The partial recovery at the end of treatment could be explained by the long period of loss of smell and taste. Similar results were found in Two Brazilian multicenter case series studies using PBMT to treat smell and taste alterations in post-COVID-19 patients. The analysis of the VAS pointed to improvement with a reduction in the scores on the scale; however, complete recovery was not observed [11, 19].
There is still no consensus in the literature regarding the ideal dosimetry and treatment protocol for fully recovering smell and taste disorders induced by COVID-19.
Panhoca et al. [12] evaluated the effectiveness of PBM in the management of anosmia and ageusia in twenty post-COVID patients, after a total of 12 sessions. There was a functional improvement in the analogue and visual scale of both smell and taste, but the maintenance of this improvement was not evaluated by the authors, as well as its impact on the patients' QoL. The authors emphasized that 12 sessions would be enough to restore the functions of smell and taste. In our study, a total of sixteen sessions were used and our patients have not fully recovered the functions of smell and taste. This fact can be justified by the longtimeof loss found in our sample.
Regarding the impact of the use of PBM on the quality of life of patients, our finding showed that the mean SF-36 subdomain scores were lower after treatment, indicating an improvement in the QoL. According to a systematic review published in 2022, one of the most common factors associated with a low level of QoL related to smell and taste dysfunction is the female sex, and the most affected and least affected domains of the SF-36 are physical role and physical function, respectively [20]. Our study agrees with the literature since our sample were mostly female, and in the pre-treatment evaluation, the least affected domain was physical function, low mean scores of QoL in several domains, including physical role.
In the evaluation of QoL after using PBM, statistical significance was observed only in the general health and social aspects domains, Despite this,in five of eight domainsof the SF-36, the scores were above 50, suggesting an improvement in the general QoL of these patients. It should be noted that, despite the statistically significant improvement in the social domain, the patients remained with scores below half, which could be explained by the partial improvement in both olfactory and gustatory functions. These results reflect the impact of the sensory loss of smell and taste on feeding, an important aspect of our social life.
Finally, we should point out that in one of the cases in this series, a patient, after improvement in both smell and taste, worsened again after 6 months. A possible explanation for this fact would be reinfection by COVID-19.
Among the limitations of this study the small number of patients caution when drawing definitive conclusions about the effectiveness of using PBMT in the recovery of smell and taste disorders. Future studies with larger samples are needed. Another limitation is that subjective assessment tests such as analogue scales are not always reliable and can lead to bias. The use of objective tests to measure smell and taste functions is most recommended for future research.
CONCLUSION
The significant and lasting improvement in smell and taste functions observed in this study suggest that photobio- modulation may be a non-pharmacological treatment option for patients with long-term COVID-19. Despite the improvements observed in our study, it is important to highlight the need for studies with larger populations in order to confirm the effectiveness of photobiomodulation in restoring smell and taste functions in patients with long-term covid.
LIST OF ABBREVIATIONS
| PBMT | = Photobiomodulation Therapy |
| VAS | = Visual Analog Scales |
| OD | = Olfactory Disorders |
| TD | = Taste Disorders |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Board (IRB) of Gaffree Guinle Hospital – Federal University of the State of Rio de Janeiro (UNIRIO) – Brazil (CAAE: 33659620.1.1001.5258).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the article's findings are recorded in the medical records of the Post-Covid neurological manifestations outpatient clinic (University Hospital Gaffree Guinle - UNIRIO, Rio de Janeiro, Brazil) and are confidential.
FUNDING
This study was funded by a research grant from Chagas Filho Foundation for Research Support in the State of Rio de Janeiro (FAPERJ).
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.