CASE REPORT
Nocardia Lymphadenitis and Encephalitis in Immunocompromised Patient: A Case Report
Rizaldy Taslim Pinzon1, 2, *, Tillandsia Filli Folia Primastuti1
Article Information
Identifiers and Pagination:
Year: 2023Volume: 17
E-location ID: e1874205X2303180
Publisher ID: e1874205X2303180
DOI: 10.2174/011874205X254011230922043119
Article History:
Received Date: 28/03/2023Revision Received Date: 26/06/2023
Acceptance Date: 17/07/2023
Electronic publication date: 30/10/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Nocardiosis-related HIV usually appears in immunocompromised patients, which is caused by Nocardia sp. Although a number of reports describe pulmonary forms of nocardiosis in HIV-positive patients, lymphadenitis and encephalitis due to this organism are rare entities. Our preliminary search has only found a few cases reported in the literature. Unless investigations like gram stain and culture for Nocardia are specifically done, the infection is often mistaken for tuberculosis. We have herein reported a case of Nocardia lymphadenitis and encephalitis in an HIV-positive patient.
Case Presentation:
A 33-year-old male presented fever, progressive weakness in the right side of the body, multiple lesions on the oral cavity, and left colli lesions. Physical examination found GCS as E4 M6 V uncounted, hypertonic and increased physiology reflexes on the right extremity without pathologic reflexes, meningeal signs, and all cranial nerves as normal. The laboratory test result was HIV-positive with CD4+ 7 cells/μL and Nocardia sp. on histopathology. A plain head computed tomography (CT) scan showed a hypodense lesion in the fronto-temporo-parieto-occipital sinistra region, and vasogenic edema. The patient was administered antiretroviral (ARV) therapy and antibiotics for nocardiosis lymphadenitis.
Conclusion:
A rare case of Nocardia lymphadenitis has been reported in this paper, and the physician must be aware of nocardiosis in HIV patients with neurological deficits.
1. INTRODUCTION
According to the World Health Organization (WHO) estimates, people living with HIV were estimated to be 38.4 million worldwide in 2021, with 36.7 million among them being adults and 650,000 people dying from HIV-related illness. HIV is one of the most common viruses causing encephalitis, followed by herpes simplex virus types 1 and 2 (HSV-1 and HSV-2), varicella zoster virus (VZV), enteroviruses, adenoviruses, parechovirus, and measles virus, although nowadays, autoimmune causes are increasingly recognized [1]. Encephalitis is a life-threatening inflammation of the brain parenchyma with neurological dysfunction conditions [2]. The worldwide incidence of encephalitis has been reported to be between 3.5 to 12.3 per 100,000 patients/year [3].
Nocardia sp. are low-pathogenic aerobic actinomycetes, which are common in the environment and rarely cause disease that usually affects immunocompromised patients [4, 5]. The most common clinical presentation findings are pulmonary. Nevertheless, extrapulmonary findings include cellulitis, lymphocutaneous syndrome, and metastatic brain abscesses [5-8]. We have, herein, reported a case of Nocardia lymphadenitis and encephalitis in an HIV-positive patient.
2. CASE PRESENTATION
A 33-year-old male was admitted to our hospital in early March 2023 with complaints of fever, progressive weakness in the right side of the body for two months, multiple lesions in the oral cavity ten days before admission, and a left mass lesion in the neck for three months, which was due to mass surgery leaving a wet wound. The patient had a history of toothache before getting a mass on the neck, progressive weight loss, and did not have any contact with patients with nocardiosis.
On admission, GCS was E4 M6 V uncounted, and vital signs showed a respiration rate of 24 beats/minute, blood pressure of 92/59 mmHg, regular heart rate of 119 beats/minute, strong pulse lift, a temperature of 38.9 oC, and oxygen saturation of 96% with spontaneous breathing of ambient air. A neurological examination found a spastic right-side weakness and speech difficulty. All cranial nerve examinations were normal.
His blood laboratory test results presented low hemoglobin, lymphocyte, erythrocyte, hematocrit, creatinine, and sodium levels; however, high basophil count, neutrophil segment, monocyte levels, and neutrophil-lymphocyte ratio have been observed. The patient got packed red cell (PRC) transfusions. Head computed tomography (CT) scan showed left side hypodense lesion in the fronto-temporo-parieto-occipital region and vasogenic edema (Fig. 1). Thorax imaging showed no abnormalities (Fig. 2).
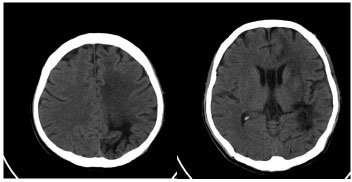 |
Fig. (1). Hypodense lesion in the fronto-temporo-parieto-occipital sinistra region and vasogenic edema on plain head CT scan. |
 |
Fig. (2). No abnormalities on thorax imaging. |
In this case, HIV was confirmed by the immunochromatographic rapid test method, and the count of CD4+ and CD8+ cells, which was, respectively, 7 cells/μL and 179 cells/μL, with a ratio of CD4+ and CD8+ being 0.04. Anti-Toxoplasma immunoglobulin and HBsAg were non-reactive. The biopsy sample of the colli lesions was taken to be tested. Ziehl-Neelsen stain procedure showed to be positive for acid-fast rod bacteria. Histopathology test showed Nocardia sp. appearance, formation of granulation, and polymorphonuclear cells to be dominant (Fig. 3).
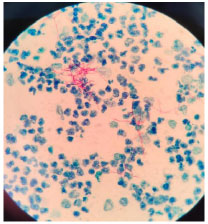 |
Fig. (3). Nocardia sp. granulation and polymorphonuclear cells observed as dominant on histopathology. |
Antiretroviral therapy (ARV) was soon administered to the patient after HIV was diagnosed. Other pharmacological therapy included cotrimoxazole (sulfamethoxazole 400 mg + trimethoprim 80 mg), nystatin suspension (100.000 IU), spiramycin (500 mg), methylprednisolone (125mg), baclofen (10 mg), vitamin B12 (3000 mcg), folic acid (1 mg), pyridoxine hydrochloride (25 mg), and paracetamol (500 mg) if necessary. Upon follow-up in June 2023, the patient showed good progress, improved consciousness, and had no additional neurological deficits.
3. DISCUSSION
Nocardia is an aerobic positive gram bacterium from the order Actinomycetales, having characteristics of weak acid stain, mycolic acid on the cell walls, and being rod-shaped, which sometimes makes it confusing to distinguish them from fungi [9]. Nocardiosis on the skin is divided into primary and secondary infection, which occurs through hematogenous spread. Primary nocardiosis of the skin is divided into subtypes, including actinomycetoma, superficial skin infection, and lymphocutaneous. Nocardia may inoculate directly via the skin and abscess or local cellulitis can be formed after skin infection. Once it has reached regional lymph nodes, it may form multiple erythematous nodules along the lymphatic tract, called lymphocutaneous nocardiosis [10]. In this case, the patient may have risk factors as a farmer. Nocardia sp. may be found in the environment, typically in dust, sand, soil, decaying vegetation, and water puddles.
Acute manifestations in the clinic, like cellulitis, lymphangitis, ulcerative/bullous lesions, linear/keloid-like lesions, and nodular-pustular lesions, are very rare, causing systemic illness [7, 11]. Lesions appear suddenly and rapidly progress as they may develop after two years of dormancy [7].
The diagnosis of this disease is confirmed by purulent culture or biopsy. Histopathologic findings include coccobacillary organisms, fibrinopurulent exudates, monocytic infiltration, granulomas, chronic nodular dermatitis, micro abscess formation, and/or sulfur granules [7]. Ziehl-Neelsen test, in this case, proved a positive acid-fast rod bacterium, caused by Nocardia sp. The histopathologic findings were the presence of Nocardia sp., granulation formation, and polymorphonuclear cells, which have supported the diagnosis.
Infection caused by Nocardia sp. is usually seen in HIV patients with less than 35 cells/μL of CD4+ count. Previous studies have confirmed the role of T-cells against Nocardia, suggesting a pivotal role in immunity [9]. As few as 7 cells/μL of CD4+ count have been reported, making it easier to get infected.
There are more than 50 species of Nocardia sp., but only 16 species are found in human infections [6]. Nocardia brasiliensis is the most common species isolated from lymphocutaneous disease [12]. Nocardia isolates have shown 88.9% susceptibility to trimethroprim-sulfamethoxazol therapy, enabling a sustained distribution to the lung, blood, and nervous system [8, 9, 13]. Other treatment options are given due to the possibility of drug tolerance; an 82.8% level of sensitivity has been proposed for amikacin, and 80.6% for imipenem. Third-generation cephalosporins, minocycline and amoxicillin-clavulanic acid, or linezolid have also proven to be effective [13, 14]. After antibiotics administration, the recovery rate of nocardiosis has been reported to be improved by 54% [9]. In this case, the patient was diagnosed with Nocardia lymphadenitis and treated with cotrimoxazole (trimethoprim-sulfamethoxazole) once a day, and then in June 2023, the patient showed a good result.
Several encephalitis manifestations include fever, alterations in behavior, cognition, personality, consciousness, deficit focal neurological function, seizures, movement disorder, and/or autonomic instability [3]. For all patients with a suspected brain infection, an HIV test [1] should be conducted, which has also been done in this case.
Brain magnetic resonance imaging (MRI) has become the gold standard for encephalitis, as it is the most sensitive and specific neuroimaging technique [1, 2]. For evaluating opportunistic brain lesions, such as toxoplasmosis, cryptococcal infection, brain lymphoma, or severe brain atrophy, CT scan with or without iodinated contrast might be used [15]. In this case, a computed tomography (CT) scan was used in emergency conditions to exclude non-hemorrhagic stroke. The fact of avascular territory in the cerebral cortex eliminates the probable state of non-hemorrhagic stroke, as shown in the CT scan for this case. However, the projection of a brain CT scan in case of a brain infection is still a question.
Cerebrospinal fluid is essential in establishing the etiology through serology, culture, and molecular methods. Lumbar puncture is an important technique for establishing evidence of central nervous system (CNS) inflammation to diagnose encephalitis and determine the management in both HIV and non-HIV patients. Several studies have not included cerebrospinal fluid (CSF) data analysis because of increased intracranial pressure concern [2], as was done in this case; however, this also constitutes a limitation of this study.
CONCLUSION
Nocardiosis is an invasive infection occurring in immunocompromised patients. In this paper, we have reported a case of Nocardia lymphadenitis and encephalitis in an HIV-positive patient. Physicians must be aware of nocardiosis in HIV patients with neurological deficits to exclude other diseases and perform early identification for good results.
LIST OF ABBREVIATIONS
| MRI | = Magnetic Resonance Imaging |
| CT | = Computed Tomography |
| CNS | = Central Nervous System |
| CSF | = Cerebrospinal Fluid |
| ARV | = Antiretroviral Therapy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Verbal informed consent has been given by the patient’s family. The identity of the patient has been kept confidential.
STANDARDS OF REPORTING
CARE guidelines have been followed.
AVAILABILITY OF DATA AND MATERIAL
The authors confirm that the data supporting the findings of this research are available with in the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.